- Reference Number: HEY-287-2023
- Departments: Plastic Surgery
- Last Updated: 31 January 2023
Introduction
This leaflet has been produced to give you general information. Some of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is Carpal Tunnel Syndrome?
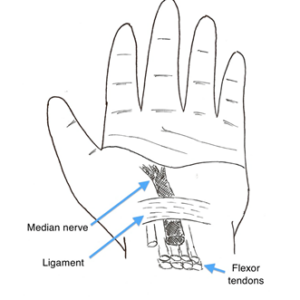
Carpal tunnel syndrome is a condition caused by one of the main nerves to the hand (the median nerve) being compressed (squashed) as it runs into the hand from the arm. This is sometimes due to thickening of a ligament running between the wrist carpal bones. The median nerve runs beneath this ligament along with the tendons to your thumb and fingers. Compression of this nerve may result in symptoms including; numbness and tingling (paraesthesia) in some of the fingers and aching pains felt in the hand and forearm. Symptoms are often worse at night but frequently affect people when they are driving, on the telephone or using their hands.
Occasionally blood tests, x-rays or nerve conduction studies (electrical tests) may be used to help diagnose or assess your condition.
Why Do I Need Treatment?
A treatment plan is tailored specifically for you, in order to help relieve or prevent your symptoms altogether. Your specific treatment options will depend on the severity of the symptoms you are experiencing.
Treatment Options
Treatment options include modifying activity, the wearing of splints, steroid injections or surgery to release the nerve. It is important to remember that, unfortunately, in some cases treatment will not relieve all of the symptoms. If a nerve is compressed for a lengthy period of time, there may be scarring within the nerve, which prevents full recovery.
Modifying activity
Some people find that certain activities provoke their symptoms. Avoiding such activities (if possible) or holding objects in a different position may reduce discomfort.
Splints
Splints are often a very effective form of treatment, particularly for those people troubled by symptoms at night. They prevent the wrist from bending whilst sleeping as this position frequently worsens symptoms. They can be worn as needed but are probably most effective when worn every night for 2-3 weeks, as this allows swelling around the nerve to settle.
Steroid injections
Occasionally steroid injections can be used to temporarily relieve symptoms. These are most useful in patients who are pregnant as symptoms often settle when the oedema (swelling) settles following the birth. Patients with thyroid disease may also benefit whilst medical treatments take effect.
Surgery
For those with severe symptoms, or symptoms not helped by splints, surgery may be beneficial. Surgery is normally performed under local anaesthetic (whilst you are awake). However, it may be performed under a regional block (injections to numb the entire arm) or general anaesthetic (whilst you are asleep). These options will be discussed with you.
A tourniquet cuff is placed around the upper arm and inflated before surgery to prevent bleeding. Although this may be uncomfortable it is usually tight for less than ten minutes. A small incision is made over the carpal tunnel to allow release of the nerve and division of the ligament. The wound is closed with sutures and a simple dressing applied. It is also possible to release the nerve by keyhole surgery through two or three smaller incisions. The results are similar whichever method is used and your surgeon will be happy to discuss the options available.
Can there be any Complications or Risks from Surgical Treatment?
Although all operations can result in complications they are infrequent (less than 1% of cases have a significant problem). It is normal for the scar to be tender for some time after surgery. You may find that the scar area becomes irritable, when pressing the hand down on a hard object, such as getting up from a chair. These uncomfortable feelings will settle quickly, but may take 3-4 months to disappear completely. It is also normal for your hand to feel weaker for about 3 months after surgery. Infection and bleeding are rare, but if they occur may require treatment; when you have your operation, you will be advised what to look out for. Severe complications such as damage to the nerve which could cause numbness or weakness are very uncommon. Approximately 1 in 3000 patients develop a painful, stiff, swollen hand known as a complex regional pain syndrome after carpal tunnel surgery.
What will happen if I need Surgery?
The waiting list office will arrange the details of your admission. You may be in hospital for up to 4-6 hours so you may wish to bring a book. You will be admitted by the nursing team and will also meet the surgeon to talk to about the operation again. They will ask you to sign the consent form, when you understand the procedure and its benefits/risks. You will be asked to change into a hospital gown and be taken into the operating theatre. The tourniquet will be fitted and the local anaesthetic injection performed before your hand is cleaned and the operation performed. The whole procedure will take approximately 30 minutes. You will be free to leave after a short period in the recovery room.
What Happens Afterwards?
You will be given a leaflet entitled ‘Carpal Tunnel Syndrome: What to Expect Following Surgery’. Simple paracetamol and anti-inflammatory tablets are usually sufficient painkillers if you are able to take them.
The aim of surgery is to relieve completely the symptoms of the condition. You may experience pain during the night and tingling sensations in your hand. These symptoms should usually disappear within a few days. It usually takes about 3 months to regain full strength but the hand can be used for light activities from the day of surgery onwards. In severe cases, numbness and muscle wasting may take months to improve and sometimes these symptoms will not disappear completely.
This leaflet was produced by the Plastic Surgery Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in January 2026.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

