- Reference Number: HEY-310/2023
- Departments: Neurology and Neurosurgery, Physiotherapy
- Last Updated: 30 January 2023
Introduction
This leaflet has been produced to give you information about how to care for your neck after surgery. Most of your questions should be answered by this leaflet. It is not intended to replace discussion between you and your physiotherapist or spinal surgeon, but may act as a starting point for discussion.
Your consultant spinal surgeon should have explained the operation procedure and the risks and benefits. This leaflet will provide you with information on the physiotherapy input you can expect after surgery.
If after reading this leaflet, you require further explanation please discuss this with a member of the Physiotherapy Team who has been treating you.
Physiotherapy after surgery
In most circumstances you will be reviewed by the physiotherapist on the first day after your surgery.
The physiotherapist will assess your limb movement and sensation, and will teach you a series of exercises (which are described later in this leaflet) to help you to get your neck moving.
The physiotherapist will also teach you how to get out of bed and encourage you to begin walking. You may have some attachments such as drips, catheter and drains. These do not prevent you from walking, although you may require some assistance initially.
You will also be expected to sit out into a chair for short periods from the first day after surgery.
In some cases you may be assessed shortly after surgery with a view to helping you to prepare for discharge home on the same day. Your consultant will have discussed with you before your surgery if you are likely to be a day case patient.
Exercises and advice post-surgery
The best thing you can do for your neck is to try to relax it and move it as freely and normally as possible. However, for the first few days or weeks after your operation it is normal for your neck to initially be stiff and sore. During this time you may find yourself tensing and protecting / guarding your neck as you move about.
It is important to remember that as things begin to heal and the pain settles down you should try to move freely and confidently again. It is a common belief that tensing your neck will protect it but in fact this often does the opposite and creates more pressure and can lead to ongoing discomfort.
Following your operation you should aim to get back to normal levels of activity by gradually increasing it as you are able. This can start straight away by sitting up in bed, sitting out in the chair and taking short walks. You should try to avoid long periods where your back is inactive.
It is important to strike a balance between periods of activity and inactivity. Inactivity can be just as harmful to your neck as over activity.
Lying
The most important thing when you are lying down is that you are comfortable. When you are at home some people prefer harder mattresses and others softer, you should be guided by comfort and pick what suits you.
You are free to move around in bed, and practising rolling from side to side will make transferring in and out of bed much easier.
It is important to minimise the strain on your neck when getting in and out of bed. To get out of bed, roll onto your side and swing your legs over the edge of the bed whilst pushing up with your arms. Sit on the edge of the bed for a moment before standing up.
Sitting
There is no such thing as the perfect sitting posture; this varies depending on the individual. Some people prefer to sit up straighter while others prefer sitting more slouched. You should sit in the posture that feels most comfortable for you.
Walking
When you first start walking your neck may be sore, this will improve over the first few days and weeks and is to be expected. It is important to try to walk little and often and gradually build things back up to normal. Do not worry too much about holding an upright posture; you are best to try to walk as normally as possible.
Personal Hygiene
Showers are initially better for you, especially if you are washing your hair, as you should try to avoid long periods where your neck is bent forwards. If you have concerns please discuss this with the Occupational Therapist on the ward prior to discharge.
You should keep your wound dry until your clips/stitches are removed. The nursing staff will update your discharge letter with the date your clips/stitches are due out and this will be sent to your doctor. You will need to contact your doctor to arrange an appointment for these to be removed on the date given on the discharge letter. These are usually removed by your doctor’s practice nurse.
Please monitor your wound for any signs of infection; these include leaking, redness and swelling. If you develop any of these symptoms you should call the ward or your doctor for advice.
You must wear your Thrombo-Embolic Deterrent (TED) stockings for 2 weeks from your discharge from hospital. These will reduce your risk of developing blood clots after your operation; they should be removed for bathing / showering then put back on once your legs are dry. After this time you can remove your TED stockings. The nursing staff will provide you with more information regarding TED stockings on your discharge from hospital.
If you are given a soft collar to wear, this can be removed for bathing and showering.
If you are given a hard collar to wear, this should not be removed for bathing and showering.
Pain Management
Following your surgery it is normal for you to experience some pain and discomfort as you recover. Try to not to panic about this as it is to be expected. If you are struggling with this you may need to consult with your doctor for advice. It would be better for you to take medication that allows you to gradually get back to your daily routine than to struggle and become more inactive.
Discharge Home
Prior to being discharged from hospital you will need to be able to complete your exercises, walk short distances comfortably and be able to walk up and down a flight of stairs (if you have them at home).
It is your responsibility to continue with your exercises and neck care independently and liaise with your doctor if necessary.
If you continue to have any pain, stiffness or weakness you may be referred for ongoing physiotherapy at your local physiotherapy unit.
Driving
Your driving / sitting posture should be based on comfort (please see the previous guidance on sitting). You should gradually build your sitting tolerance back up over time and take regular breaks where you get up and move about.
It is your responsibility to ensure your vehicle insurance covers you prior to commencing driving after your surgery. In some cases your vehicle insurance may be invalidated if you do not inform your insurance company about your surgery.
Lifting
Avoid lifting heavy objects and also holding items at arms length away from your body. Always use a correct lifting technique, bending at the knees and not at your back (see following diagram). Avoid bending, twisting or leaning movements.

Work
Returning to work will depend very much upon your recovery and the type of work you do. It is important that you discuss with your doctor when it is safe to return to work.
Exercises
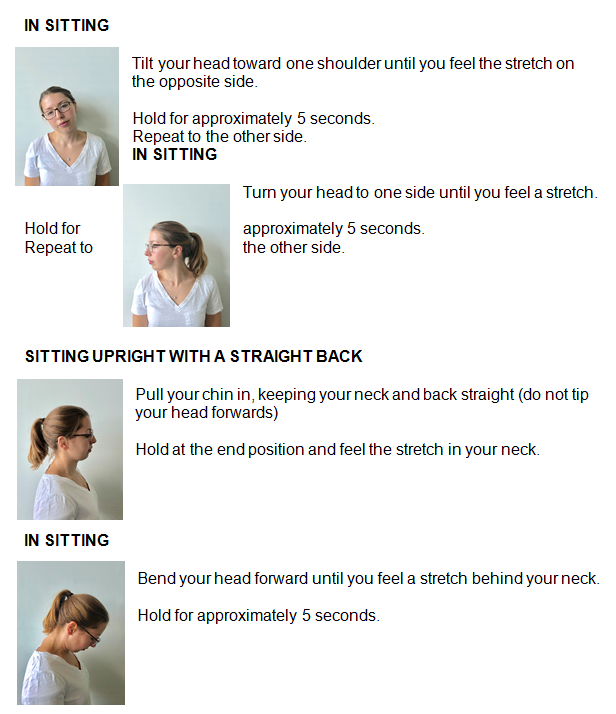
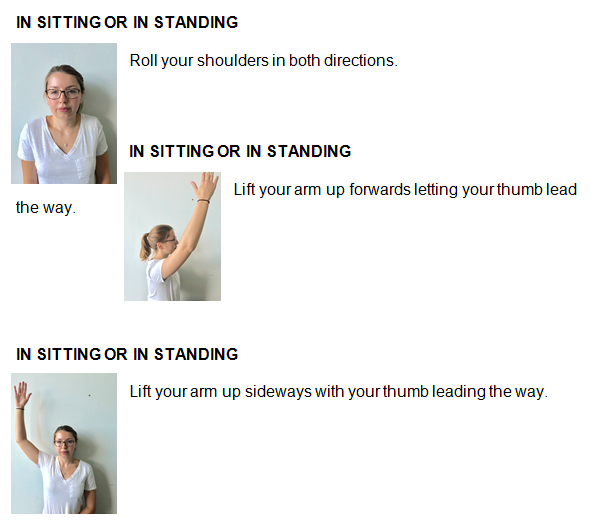
These exercises are designed to improve the movement and strength in your neck, prevent muscle spasm and help the healing process.
They should be carried out approximately three times a day. Begin by doing 2 or 3 of each exercise and gradually increase from there, aiming to build up to 10 repetitions. Remember these are gentle exercises.
If you experience any increase in pain cease from doing that exercise until the pain resolves at which point you can recommence the exercise.
It is also beneficial to increase your walking tolerance to aid general fitness. This should be done within the limits of pain.
You may also be provided with additional exercises to strengthen your neck, back, arms or legs if your Physiotherapist deems this necessary.
Collars
Following surgery you might be issued with a neck collar if your Consultant has advised this.
If you are given a soft collar for pain relief it is important that you do not become reliant upon it. You should start to remove the collar for increasing lengths of time following surgery and at approximately 6-8 weeks remove all together. It should also be removed in order for you to carry out your exercise program.
If you are issued with a hard collar following surgery it should be worn day and night until your Consultant advises you to remove it. It should not be removed to do your exercises.
In some instances the Spinal Surgeon may advise differently, please follow their instructions.
Telephone follow-up service
Your Consultant may place you onto the telephone follow-up service if required.
This is when you are expected to recover well with time and you do not routinely need to see the Consultant for follow-up review in person.
The Physiotherapists will arrange this follow up with you on your discharge from hospital, and make provision to track your progress by telephone.
This leaflet was produced by the Neuro-Orthopaedic Physiotherapy Team, Hull University Teaching Hospitals NHS Trust and will be reviewed in January 2026.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

