- Reference Number: HEY1107/2023
- Departments: Orthopaedics, Physiotherapy
- Last Updated: 1 May 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a Total Hip Replacement?
A total hip replacement (THR) is a common orthopaedic surgery where the damaged hip bone and cartilage is removed and prosthetic components are inserted. This is most likely to occur following a fall/injury which has resulted in a hip fracture.
Why do I need a Total Hip Replacement?
Following discussion with your doctor they may have advised a total hip replacement. You may have been offered a THR to:
- Relieve pain from the damaged hip joint.
- Increase quality of life.
- Improve the function of the hip joint.
- Increase mobility.
This leaflet is intended to help you reach a decision by outlining the operation, risks, benefits and outcome of a hip replacement. The content of this leaflet is not intended to be a comprehensive list or replace the discussion between you and the surgeon or your doctor, but rather is a brief guidance to the degree of benefits and risks that you need to consider.
Can there be any complications or risks?
Risks and complications of this surgery can include:
- Clots – to reduce the risk of blood clots, you will be assessed for and given blood-thinning medication.
- Stroke/heart attack/heart failure – these can happen and unfortunately the stress of surgery can increase the risk of such events occurring.
- Swelling – swelling may persist for up to 3 months post-op. To reduce swelling, rest the leg for an hour or so.
- Nerve/Blood vessel damage – the blood vessels (0.1%), or the nerves (1%) which allow you to feel or move your leg, may get damaged. The healthcare team will monitor you closely for any indicators including; discolouration, changes in temperature, weakness or severe numbness.
- Infection – there is a risk of infection, please report any wound leakage, redness, heat, increasing pain and/or discharging pus.
- Leg length discrepancy – occasionally following hip replacement there can be a difference in your leg lengths, these can normally be fixed with the help of orthotics.
- Dislocation – there is a slight risk of dislocation occurring, to reduce the risk of dislocation: follow hip precautions and complete exercises to help strengthen the soft tissues surrounding the hip.
- Loosening – with time the prosthetic might wear out and you might require further surgery.
How do I prepare for the surgery?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this procedure.
What will happen?
Following your injury you are likely to be admitted to the hospital via A&E where you will be assessed and admitted onto a ward.
Upon being transferred onto the ward, the team will admit you, they will take note of your; reason of admission, clinical diagnosis, past medical history, social history and any other details deemed relevant.
Your consultant will review your case and decide on the best surgical option for you. They will have a conversation with you regarding why they have chosen this and explain the risks and benefits. You will then be asked to sign a consent form.
Before you go to surgery, you will have a pre-operation assessment. The nursing team will run a variety of tests, include a MRSA and COVID-19 swab, blood tests, ECG and potentially further x-rays.
The staff will run through a checklist prior to taking you to the operating theatre. An anaesthetist will assess you for the anaesthetic. You will also be formally assessed for your risk of developing blood clots.
Exercises
Whilst you are awaiting surgery, the therapy team will encourage you to complete some bed exercises.
Evidence has shown that preoperative rehabilitation can help reduce the length of hospital stays for people having a hip replacement. Exercises help to increase circulation and strengthen muscles.
Complete the following exercises on the unaffected side. On the affected side, complete the ankle exercises as pain allows and focus on upper limb range of motion and strength.
Complete these exercises throughout the day whilst awaiting surgery and post-op as pain allows.
- Ankle Pumps – slowly push your foot up and down. Complete 3 sets of 10.

- Knee Flexion/Extension – slide your foot toward your buttocks, bending your knee and keeping your heel on the bed then straighten your knee back out and press it down into the bed and hold for approx. 3-5 seconds. Complete 3 sets of 5.

- Straight Leg Raise – Tighten your thigh muscle with your knee fully straightened on the bed and then lift your leg several inches. Hold this for 5 to 10 seconds. Complete 3 sets of 5.

What to expect
- Your leg will be ‘marked’ for the operation by drawing an arrow pointing to your hip.
- You are not allowed to eat or drink from midnight prior.
- You are likely to be off the ward for approximately 2-6 hours although the procedure normally take 60-90mins.
- When you wake, you will be in a recovery area where you will be monitored to ensure you recover well immediately post-op.
- You will then return to the ward following this where you will be assessed by physiotherapy and occupational therapy the following day.
Therapy Questionnaire
The therapy team will ask you to complete a questionnaire with them about your social history. This is used to determine your set up at home and any support/equipment you might already have in place. For example:
- Who do you live with?
- Is this in a house/bungalow/flat?
- What is the access like? (Any steps or rails?)
- How were you mobilising pre-op? Were you using any walking aids?
- How were you managing? Did you need family support or a package of care?
- Do you have any equipment in situ? Anything to help you in/out of bed or on/off the toilet?
Surgery
- An incision (of up to 30cm) will be made over the side of your hip.
- Part of your femur head/ broken ball of the hip is removed and the shaft of your femur is hollowed out.
- A new socket is fitted into your pelvis.
- A metal shaft (stem) with a ball on its upper end is placed into the hollow of your femur.
- The stem and socket may be fixed with bone “cement”.
What will happen afterwards?
Post-operation you will be working with physiotherapists and occupational therapists on a daily basis within the hospital. Hip patients are normally mobilised within first 24 hours, whether this just be sitting of the edge of the bed or getting out into the chair.
Post-op you will be allowed to put as much weight on your operated leg as you can tolerate (unless otherwise stated by your surgeon/physio).
You are likely to need a walking aid to help you mobilising for the first 6 weeks post-op, your therapists will help you to progress as appropriate.
Hip Precautions
Due to the incision made during surgery, the surrounding muscles will be weak and need time to heal. For 6-8 weeks post-operation, it is important to avoid certain movements in order to reduce the risk of dislocation.
- Do not bend your hip more than 90 degrees.
- Avoid bending down to the floor, this means you will need help/aids to complete lower half personal cares e.g. washing shins and feet.
- Do not cross your legs, or ankles in lying, sitting or standing position.
- Do not sit on low furniture or attempt to get into the bath or drive.
- Try to avoid twisting/turning from your waist/hip.
One of the hip precautions is ‘do not sit on low furniture’ as such the therapy team will need to gather some furniture heights to ensure that the furniture at home is suitable. The therapy team will ask you or a family member to measure; the bed (compressed i.e. sat on), a chair (compressed) and the toilet.
If these are too low then the therapy team will suggest ways to raise these/provide equipment to raise them.
Physiotherapy
The rehabilitation routine has four components: therapeutic exercise, transfer training, gait training, and instruction in the activities of daily living.
The physiotherapy team will aim to see you day 1 post-operation to assess you. The aim is to; regain functionality and independence and to minimize complications such as; infection, deep vein thrombosis, pulmonary embolism, and dislocation.
The physio will look at;
- Circulation and sensation
- Range of motion in upper limb and both legs
- Muscle power
- Functional movement
- Establishing a safe transfer method using appropriate aids (e.g. Zimmer frame / crutches)
The therapy team will aim to see you every day you are on the ward to progress your mobility and transfers.
Safe Technique to Stand/Sit
- When standing, take the majority of the weight through your ‘good’ leg and push up from the bed/chair with your arms, gain your balance and then take a hold of the walking aid.
- If using a transfer aid you can pull up on them as instructed.
- DO NOT pull up on walking aids, as they are unstable and can tip over.

- When sitting, wait until you can feel the chair on the back of your legs and then reach for the chair arms. As you sit down, slide your operated leg out and slowly lower yourself down.
- When sitting make sure to slide your leg in order to maintain your hip precautions.
There is a range of aids used on the wards to help facilitate patients transfer and mobilise. Some aids (Sara steady/molift) assist you in transferring and reduce the need for stepping; these might be used if you are in a lot of pain. Other aids include; zimmer frames, gutter frames and crutches.
Your physiotherapist will assess which aid will be the safest and most appropriate for you to use. The physio team will then try to progress you back to your baseline mobility.
The following sequence should be used:
- Move the walking aid slightly ahead of you. Ensure the whole aid is on the floor.
- Step your operated leg forward and push down through the aid with your arms.
- Move your good leg forward so that it is in line with your operated leg.
Repeat these steps – 1) walking aid, 2) operated leg, 3) good leg – to continue walking.
To aid in your rehabilitation, it is important that you continue with the exercises shown previously. Your physiotherapy team may also advice you of further exercises to complete. Prior to discharge, if you are going home, the physio will need to assess you completing the step/stair assessment to ensure you are able to manage this safely prior to leaving the hospital.
If you cannot manage this, don’t worry – there are lots of options we can discuss.
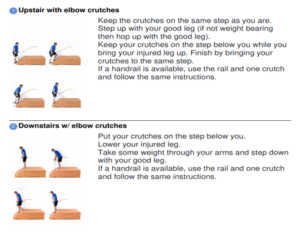
There is a simple sequence to mastering the step/stairs.
Occupational Therapy
Occupational therapies focus more on the functional activities and activities of daily living. Due to the hip precautions you will need to follow you will need to adjust how you approach some activities e.g. how to dress using equipment in order to avoid bending down.
As mentioned earlier you will be given a minimum furniture height (your leg length + 2inches) in order to maintain the hip precautions, if these are not suitable the therapists will advise you on the next steps. It is likely that you will definitely need some equipment to raise the height of your toilet.

Washing and Dressing
In order to maintain your hip precautions you will need to adjust the way you wash and dress.
- You must not use the bath; if a shower is not available, we would recommend strip washing at the sink.
- The therapists will teach you a new technique using long-handled dressing aids.
- Dressing aids are essential to reduce risk of dislocation; unfortunately, these will need to be purchased privately.
Kitchen Activities
You will also need to reconsider the layout of your kitchen.
- Place commonly used items on the worktop so that you do not have to bend to access items.
- Try to avoid using the oven, as it requires bending down.
- You will need to consider how you are going to get your shopping. Can family support? Can you order it online?
Domestic Tasks
Following the operation, you are likely to need help with housekeeping, laundry and cleaning due to walking aids and the need to follow hip precautions.
Recovery
Following surgery, the average length of stay is recorded as 5 days, however patients can be discharged from day 3. Elective patients can potentially be discharged same day.
- Day 1: get up with therapists, you might need to use an aid e.g. Zimmer frame or crutches.
- Day 5: potentially be discharged e.g. to a rehab bed or home with support
- 4 to 6 weeks: start feeling stronger and to be able to get around with less pain.
- 6 weeks: start returning to work and completing light activities of daily living.
- 4 to 6 months: you should be functioning well however weakness in the muscles surrounding your hip may persist for up to 2 years.
Everybody recovers at differing speeds and this will depend upon your general health and wellbeing before your injury, the nature of your surgery, and other individual factors.
Discharge
When the doctors are happy that you are medically fit and you can leave the hospital, the therapy team will discuss the different options with you depending on your individual needs:
- Home with equipment/support
- Rehabilitation bed (short-term rehabilitation service)
- If discharge home or to a rehabilitation bed are not suitable for your needs, the ward team will involve social services to support in making the right decision for you
Once you and the team have made a decision, they will organise your discharge.
Ongoing referrals
Following your discharge from hospital, you may require further therapy input, with your consent the therapy team will make the relevant referral to help you progress at home.
- Community physiotherapy
- RAFT – Rehabilitation and Acute Falls/Trauma Therapy Team (for those in the catchment area)
- MSK – Musculoskeletal
You are also likely to have a follow-up appointment, this will be specified in your post-operative note and you will receive an appointment letter through the post.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Trauma Orthopaedic Department via telephone:
Ward 12, Floor 12, HRI: 01482 675012
Ward 120, Floor 12, HRI: 01482 675120
Visiting Hours: open visiting between 11am-7pm
Useful Numbers
City Health Care Partnership single point of access number 01482 247111 (ask for the ICT team regarding rehabilitation)
Social Services (Hull) 01482 300300
Social Services (ER) 01482 393939
NRS (Equipment) 03448936375
British Red Cross 01482 499837
Home from Hospital 01482 447673
This leaflet was produced by the Trauma Orthopaedic Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in 08/2025
All photos with kind permission of ©Physiotec™ and ©Healthcare Pro
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

