- Reference Number: HEY-173/2018
- Departments: Maternity Services
- Last Updated: 18 July 2018
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor or midwife but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team. If a baby is found to be in a breech position at 36 weeks, it is usual to refer you to the hospital to discuss options for the birth.
What is a Breech position?
A breech position is when your baby is lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position a. Breech is very common in early pregnancy, and by 36–37 weeks of pregnancy, most babies turn naturally into the head-first position as the baby is getting ready to be born. Towards the end of pregnancy, only 3–4 in every 100 (3–4%) babies are in the breech position
Your breech baby may be lying in one of the following positions:
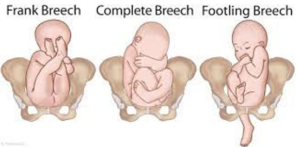
Extended or frank breech – the baby is bottom first, with the thighs against its chest and feet up by its ears. Most breech babies are in this position.
Flexed or complete breech – the baby is bottom first with its feet right next to its bottom. The thighs are against its chest and the knees are bent.
Footling breech – when one or both of the baby’s feet are below its bottom.
What if My Baby is Breech Towards the End of My pregnancy?
If your baby is breech at 36 weeks of pregnancy, your healthcare professional will discuss the following options with you:
- trying to turn your baby in the uterus into the head-first position by external cephalic version (ECV)
- planned caesarean section
- planned vaginal breech birth.
What is External Cephalic Version (ECV)
Your obstetrician or midwife may advise trying to turn your baby into a head first position. This technique is called external cephalic version (ECV). This is when gentle pressure is applied on to your abdomen which helps the baby turn in the womb to lay head first. ECV is usually performed after 36 or 37 weeks of pregnancy. However, it can be performed right up until the early stages of labour.
What is the main Benefit of ECV?
The main benefit to ECV is that it increases the likelihood of having a normal birth (head first). Successful ECV lowers your chances of requiring a caesarean section and its associated risks.
Does ECV always Work?
ECV is successful for about half of all women. Your obstetrician or midwife will provide you with information about your own individual chance of success. Relaxing the muscles of the womb with medication during an ECV is likely to improve the chances of success. This medication will not affect the baby. You can help by relaxing your abdominal (tummy) muscles.
If your baby remains breech, your choices may include a:
- Caesarean delivery – this is a surgical operation where a cut is made in your lower abdomen to allow your baby to be delivered. Caesarean delivery carries a slightly higher risk for you, compared with the risk of having a vaginal breech birth. Caesarean delivery does not carry any long-term risks to your health outside of pregnancy. However, there may be long-term effects in future pregnancies for either you and/or your babies.
- Vaginal breech birth – There are benefits and risks associated with both caesarean delivery and vaginal breech birth and these should be discussed with your obstetrician and/or midwife. This will help you decide the best plan for you and your baby. A vaginal breech delivery may not be recommended as safe in all circumstances. It is a more complicated birth, as the largest part of the baby is last to be delivered and in some cases this may cause difficulty.
Is ECV safe for me and my baby?
ECV is generally safe and does not cause labour to begin. The baby’s heart will be monitored before and after the procedure.
Like any medical procedure, complications can sometimes occur. Immediately after ECV, there is a 1 in 200 chance of you needing an emergency caesarean section because of bleeding from the placenta and/or changes in your baby’s heartbeat and it is for this reason that the procedure is carried out on the Labour Ward at the Women and Children’s Hospital where the baby can be delivered by emergency caesarean section if necessary. Harm to the baby is unlikely.
These are a few reasons you would not be suitable for an ECV:
- Caesarean section is required for other reasons
- Recent bleeding
- Baby’s heart rate tracing (also known as a CTG) is abnormal
- Your womb is not the more usual pear-shape
- Your waters have broken
- Twin pregnancy
- Small baby
- Pre-eclampsia
Attending your appointment
There are no restrictions on food or drink before you attend your appointment, on the Labour Ward. Feel free to come with your partner or a companion. We aim to complete the procedure without delay but please be aware that if the Labour Ward is busy you may need to allow several hours for your visit.
Please bring along your hand held pregnancy record and something to do or listen to, in case you have to wait.
What will happen?
You will attend the Labour Ward on the 2nd floor of the Women’s and Children’s Hospital on our Hull Royal Infirmary site. Upon arrival you will be met by a member of staff who will show you into a single room. A midwife will care for you and keep you fully informed on what will happen. The midwife will undertake a number of health checks which will include:
- Taking your blood pressure
- Pulse and other vital signs
- Monitoring the heart rate on a CTG
You will be seen by an obstetrician who will explain the procedure and scan your baby. They usually recommend an injection of a medication called Terbutaline® which is given under your skin. This medication helps to relax the muscle in the uterus and increases the chance of the baby turning successfully. This medication does not affect the baby however it may make you feel a little shaky and make you aware of your heart beating faster. These effects wear off very quickly (within an hour or two).
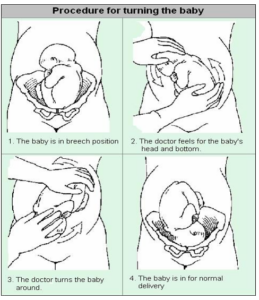
The obstetrician will use their hands to gently encourage the baby to turn around. You can help by relaxing your tummy muscles (ECV can be uncomfortable but should not be painful). Please try to tolerate the procedure as long as you can to increase the chances of turning your baby to a head first position. If you are experiencing pain please tell the obstetrician so they can move their hands or stop. Sometimes the baby’s heart rate can slow down during the procedure. Please do not worry this is only temporary and the midwife and obstetrician will be observing you and baby closely.
What happens afterwards?
Once the procedure has been completed successfully, your midwife will monitor the baby’s heart rate for a further 20 – 30 minutes. During that period, it will be documented in your antenatal notes and on our electronic record (Lorenzo). Some women feel some slight discomfort if the procedure was successful however some women report feeling more comfortable because babies head is no longer under the rib cage. If ECV is successful, there is still a small chance that your baby will turn back to the breech position. However, this happens to less than 5 in 100 (5%) women who have had a successful ECV.
If the procedure has not been successful then the obstetrician will discuss a choice of delivery and agree a plan of management with you. It is possible to have another attempt at ECV on a different day.
If you are 1 of the 16 pregnant women in 100 (16%) who are rhesus negative you will be offered an injection of anti-D before you are sent home.
Following the procedure you should contact the hospital and speak to a midwife who will be able to advise you should any of the following events occur:
- Any vaginal bleeding
- Severe pain
- Reduction in babies movements
- Contractions
- If your waters break
Should you require further information or advice please contact Hull and East Yorkshire Women and Children’s Hospital
Important telephone numbers:
Antenatal clinic (01482) 382623
Antenatal Day Unit (01482) 382729
Labour and Delivery Suite (01482) 604490 (01482) 604390 (01482) 607860
Community Midwives (01482) 382658
Useful Contacts
You may wish to find out other information about external cephalic version, examples include:
http://www.rcog.org.uk/
http://www.womens-health.co.uk
http://www.infochoice.org
Breech presentation and turning a breech baby in the womb (external cephalic version). Patient information leaflet
To be updated March 2026
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

