- Reference Number: HEY-1341/2022
- Departments:
- Last Updated: 1 December 2022
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a Volar plate?
The volar plate is a strong ligament, not visible on x-ray, at the palm side of the middle joint of your finger. This structure supports the middle joint and prevents it being overstretched backwards or dislocated. The volar plate can be partially or fully torn and may sometimes pull off a small piece of bone (avulsion) when it is damaged.

How should it be treated?
This injury can be treated with neighbour strapping, when the injured finger is taped to the finger next to it, for 2 weeks. The strapping will provide the finger stability, whilst still allowing and encouraging movement.
To manage your pain, we advise that you regularly take simple pain relief, which can be bought over the counter. If you have allergies or conditions, which prevent the use of pain-relieving or anti-inflammatory medication, please seek advice from your doctor or a pharmacist.
Extra strapping can be purchased from your local chemist and should be replaced when it becomes wet or worn. Please ensure it is applied above and below the finger joints, so that it does not restrict movement as this will cause stiffness.

It is important to note that smoking will delay the healing process and so should be minimised if at all possible.
What should I do in the first few days?
It is normal for the hand to be painful and swollen following this injury, sometimes even spreading to parts of the hand that were not injured. However, although a normal reaction, swelling which stays in the fingers too long, becomes very dense and sticky (fibrous) and can result in long term stiffness.
- Allow your hand to rest slightly for the first 48 hours
- Take over the counter pain relief such as paracetamol
- Keep your hand elevated above your heart to reduce swelling
- Move all of the uninjured fingers fully and often to prevent stiffness and reduce swelling.
- Avoid bending your finger backwards at the injured joint.
- Use your hand as normally as possible, as your comfort allows, for daily tasks such as dressing, eating meals etc.
You can remove the strapping yourself at 2 weeks. No further X-ray will be needed.
Exercises
Complete rest is not advisable. Whilst in the strapping, it is important that you try to use your wrist and hand normally when doing everyday tasks like washing, dressing and eating.
Exercising the hand early is very important to prevent stiffness at the finger joints.
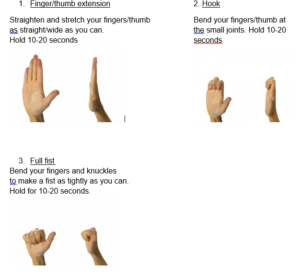
The following exercises should each be repeated 10 times and completed every 2-3 hours. Support your elbow on the table with your wrist straight.
When can I drive again?
You may not be insured to drive whilst the strapping is in place. It is advisable to check with your insurance company.
It may be safe to return to driving when
- You are no longer required to wear the strapping
- You can comfortably operate all the hand operated controls such as steering wheel, handbrake, and gear stick.
- You can perform an emergency stop.
What about work and sport?
You can return to work or school as soon as pain allows and you can do your normal duties. You may be able to work with your strapping on, but this will depend on your job.
Full contact sport should be avoided for at least 6 weeks.
When should I call for a PIFU?
It may take several months for discomfort to settle, and the finger or thumb may appear ‘thicker’ than on your other hand. This is normal.
You should initiate a PIFU appointment if:
- Pain and swelling is getting significantly worse
Or if after 2 weeks of exercise you are unable to:
- Fully straighten your finger, or you feel your finger is becoming increasingly bent.
- Make a fist, or get your fingertip to your palm.
- You are struggling with light daily tasks.
Or after 4 weeks, you are struggling to return to your usual work or hobbies.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Physiotherapy Department on telephone: 01482-624880.
This leaflet was produced by the Physiotherapy Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in June2025
Ref: HEY1341/2022
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

