- Reference Number: HEY748-2023
- Departments: GI Physiology, Paediatrics
- Last Updated: 30 November 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
If after reading this leaflet you have any concerns then please feel free to contact the Department of GI Physiology on tel: 01482 624036.
What is 24-hour pH and impedance monitoring study?
Your child has been referred for a 24-hour pH and impedance monitoring study. The study will measure the amount of fluid coming up (refluxing) into the oesophagus from the stomach over a 24 hour period and if this fluid is acidic. This allows us to establish whether your child’s symptoms could be due to reflux.
Why does my child need 24-hour pH and impedance monitoring study?
This study provides valuable information regarding your child’s condition and can help to decide what the best treatment is for them. Unfortunately, there are no other less invasive tests available that will give us this information.
Can there be any complications or risks?
Complications or risks are minimal during the insertion of the 24-hour pH and impedance probe. A runny nose, sneezing, nasal discomfort and a sore throat occasionally occur. There is a small radiation dose with the X-ray that is required to check the 24-hour pH and impedance probe position.
How do I prepare my child for the 24-hour pH and impedance monitoring study?
Your child cannot have anything to eat for 4 hours prior to the study*. However, they may drink water up to 2 hours before the study*.
*If your child is diabetic, please call the department for advice.
It is important that your child stops taking any of the following medications:
7 days before the study
Any proton pump inhibitor such as:
- omeprazole (Losec)
- lansoprazole (Zoton)
- rabeprazole (Pariet)
- esomeprazole (Nexium)
- pantoprazole (Protium)
3 days before the study:
Any Histamine H2 receptor antagonist or drugs listed here:
- cimetidine (Tagamet)
- nizatidine (Axid)
- famotidine (Pepcid)
- domperidone (Motilium)
- mebeverine (Colofac)
- alverine citrate (Spasmonal)
- buscopan or baclofen (Lioresal)
- metoclopramide (Maxolon)
On the day of the study:
- No antacids (i.e. Gaviscon)
What will happen?
Please bring your child to the Children’s Outpatients Department, which is situated in the Women and Children’s Hospital at Hull Royal Infirmary.
When you have informed the receptionist that you have arrived, a member of staff from the Department of GI Physiology will come and explain the study to you. A fine tube with small sensors will be passed via your child’s nose into their stomach, then moved into the oesophagus (food pipe). Once the tube has been positioned correctly, it will be secured with some tape to the side of your child’s face. The end of the tube is passed under the clothing and will be attached to a recording device that can be carried around in the small shoulder bag provided. A member of the GI Physiology team will explain how to use the monitoring equipment during the study.
Your child will be required to attend the X-ray department to confirm that the tube is in the correct position. Your child will need to return to the Children’s Outpatient Department where the X-ray will be reviewed by a member of the GI Physiology team. If necessary, small adjustments will be made to the position of the tube. After the study has started, your child may go back to school or home.
Placement of 24-hour pH and impedance probe:
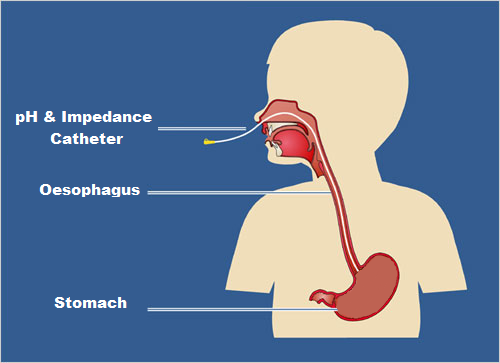
Diagram produced by Hull University Teaching Hospitals NHS Trust
What happens afterwards?
Please be aware that your child will be required to come back to hospital the following day to have the tube and the recording equipment removed (location and time to be agreed). We would expect you and your child to be at the hospital no longer than 15 minutes (on day 2) before you are able to go home. Your child should not experience any problems after the test, however please contact the department if you have any concerns.
The results of the test will be analysed before a diagnosis can be made. Once this is complete, the report will be sent to the consultant in charge of your child’s care. They will decide what the most appropriate treatment is. You should expect to hear from the hospital within 6 weeks of having the test. If you have not heard from the hospital within 6 weeks, please telephone the hospital on tel: 01482 875875 and ask to speak to the secretary of the consultant caring for your child.
Should you require further advice on the issues contained in this leaflet, please contact the Department of GI Physiology on tel: 01482 624036.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats your child, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to your child. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your child’s condition, the alternatives available for your child, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about your child
We collect and use your child’s information to provide your child with care and treatment. As part of your child’s care, information about your child will be shared between members of a healthcare team, some of whom you may not meet. Your child’s information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide your child with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your child’s doctor, or the person caring for your child.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about your child. For further information visit the following page: Confidential Information about You.
If you need information about your child’s (or a child you care for) health and wellbeing and their care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

