- Reference Number: HEY1080/2022
- Departments: Radiotherapy
- Last Updated: 1 June 2022
Introduction
This leaflet has been produced to give you general information about your External Beam Radiotherapy EBRT. This leaflet should answer most of your questions. It is intended to add information to the discussion between you and the healthcare team, and may act as a starting point for discussion. If after reading it, you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is External Beam Radiotherapy EBRT?
EBRT is the use of high energy X-rays to treat cancer. It works by causing damage to the cancer cells in the treatment area. Although some normal healthy cells are also damaged, these are able to recover and repair themselves. It is delivered using a machine called a Linear Accelerator or Linac for short. The picture shows the two different types of linear accelerators we have within the department. We will refer to External Beam Radiotherapy as “EBRT” throughout this leaflet.
Figure 1 Linear Accelerators, Radiotherapy department pictures
EBRT does not make you radioactive and you are safe to be around others (including children) whilst you are having treatment. For more information, please refer to the leaflet ‘Introduction to Radiotherapy Treatment’ or speak to a member of your Healthcare Team.
EBRT treatment is commonly used in cancer treatment. It may also be combined with other treatments including Surgery and/or Systemic Anti-Cancer Therapy, (SACT). Before you start your treatment, your clinician will discuss your treatment options with you and ask for your consent.
Systemic Anti-Cancer Treatment (SACT) (Chemotherapy) and EBRT
If you are undergoing SACT, treatment along with EBRT you may be required to attend for SACT treatment before you can start your EBRT. You may also be having SACT at the same time as your EBRT. Your clinician will discuss this with you if it is necessary.
Planning your EBRT
EBRT is designed individually for each patient so before you can start we will need to plan your treatment. This will mean a visit to our CT scanner for an EBRT planning scan so we can plan your treatment. This will be at the Queen’s Centre at Castle Hill Hospital.
Using the scans from your CT, the Radiotherapy Planning Team will work with your clinician to create a personalised treatment plan based on the precise shape, size and location of the tumour. If your treatment is after your tumour removal surgery, then we will take scans to examine the area where the tumour was removed.
For more information, please refer to the leaflet ‘Introduction to Radiotherapy CT Planning’.
Radiotherapy CT Scanner
Radiotherapy Department Photograph
For this CT planning scan, you will be positioned comfortably on the couch, It is important that you are comfortable as this will be the position you will be in for your daily treatment. If you are not comfortable, please inform a member of staff at the time so adjustments may be made.
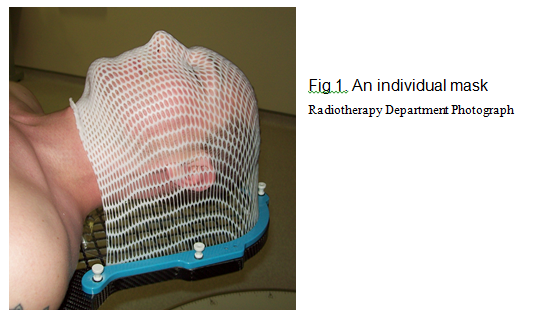
Your first appointment with the radiotherapy department will be for an individual mask, (Fig. 1), to be made and for a CT planning scan. A member of staff will discuss the procedure and gain your consent at the start of your appointment. Your mask will be made of a special plastic that becomes flexible when warm. Whilst some may find this procedure uncomfortable, your mask is very important as it will be used everyday to keep you in the correct position for your treatment. It also avoids the need for drawing marks on your skin. It will take approximately 15-20 minutes to make your mask, after which you will have a CT planning scan in your mask. This will typically take around 10 minutes.
What happens during my treatment?
A member of staff will escort you into the treatment room and ask you your name, date of birth and address for identification purposes.
The treatment machines and rooms are very large and can appear quite overwhelming when you see them for the first time. You may need to partly undress and put on a gown, or just expose the area of treatment once on the treatment couch; the therapeutic radiographers will discuss this with you when you first attend the department. Once inside the treatment room you will be assisted into the correct position for treatment on the couch. This will be the same position you were in when you had your CT planning scan. The therapeutic radiographers will place your mask on you and will check that your position is correct for treatment. You will then, be moved nearer the treatment machine and the staff will then leave the treatment room to switch on the Linac. You will only be alone for a few minutes. The therapeutic radiographers are watching you on the closed circuit TV (CCTV) monitor, throughout treatment. This image is not recorded or stored; it is purely for patient safety. During treatment, you will not see or feel anything apart from the couch and possibly the machine moving into position and a buzzing noise whilst the external beam radiotherapy is being delivered.
Review appointments during treatment
You will have regular reviews with the therapeutic radiographers and/or radiotherapy nurses as you progress through your treatment. Please be honest with your answers as they can offer advice to ease any side effects that you may be suffering. If necessary, they may be refer you to our on call medical team for their assistance.
Side effects (leaflet dependent):
Radiotherapy causes damage to you body’s healthy cells only within the treatment area, as well as cancer cells, and as a result, you may experience some side effects from your treatment. If you have any concerns, please ask one of the therapeutic radiographers or radiotherapy support team within the department.
EARLY SIDE EFFECTS:
These can happen during the course of, or within 3 months of finishing your radiotherapy treatment. If they occur during your course of EBRT, please inform the therapeutic radiographers or nurses, as they can advise you how to reduce the effects. If you have finished your treatment, please contact your GP.
Worsening of symptoms
Radiotherapy can cause swelling of the brain and this can cause symptoms to become slightly worse. These may include headaches, weakness of the limbs, increase in seizures, speech or memory problems.
Skin
Your skin, within the treated area, may become discoloured and itchy. To help your skin feel better you should wash the area gently. Use a soft towel and pat the area dry, do not rub. Skin reactions can get worse for a week or two after the external beam radiotherapy is finished and you should continue to follow the advice given by the therapeutic radiographers or member of the radiotherapy support team. The treatment area will be sensitive to the sun during treatment and continue to protect the treated area from the sun for at least one year after you have finished treatment. Because your skin will be more sensitive, we advise you use sunscreen with SPF 50.
Hair loss
Only hair in the treated area will stop growing and may fall out. At your treatment consent, a member of the clinical team will tell you if you might lose your hair. Sometimes hair will not grow back after treatment.
Fatigue/Tiredness
Radiotherapy can make you feel tired so it is important to rest as much as you feel you need, but you are encouraged to maintain some gentle exercise. It is important to drink plenty of fluids, approximately 2 litres of water a day. We do not recommend alcohol.
Nausea/Vomiting
Radiotherapy may make you nauseous (feeling sick) or be sick (vomit). This is more likely if the treatment area is near the stomach or the brain. If this occurs, please tell the therapeutic radiographers for help and advice. They may arrange for you to see the radiotherapy support team as it is usually possible to control this with medication. If you do not feel like eating, try to maintain your fluid intake.
LATE SIDE EFFECTS:
These can occur many months to years after your radiotherapy has finished. These late side effects are hard to predict and can unfortunately be permanent, these will be written on your consent form after your discussion with your clinician.
These can occur many months to years after your radiotherapy has finished. These late side effects are hard to predict and can unfortunately be permanent, these will be written on your consent form after your discussion with your clinician.
What happens when I finish treatment?
Once you have completed your course of radiotherapy treatment, you will receive a follow-up appointment with your clinician; it may be a telephone consultation. You will receive the appointment through the post. This is usually around 2 – 6 weeks after treatment has finished, allowing any side effects experienced to settle down.
USEFUL INFORMATION AND CONTACTS
The information provided in this leaflet should have answered most of your questions. If you have any further questions, please ask any member of your healthcare team.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Radiotherapy Information and Support Team
(01482) 461206 Email: hyp-tr.radiotherapy.information@nhs.net
RESEARCH
Hull University Teaching Hospitals NHS Trust is a research-active Trust with a research strategy that includes cancer treatment and care. The radiotherapy department participates in national and international research studies to improve treatments to make them safer, more effective and to reduce side effects. We also develop patient-centred local research to improve your radiotherapy experience to benefit you and your family. We would like to encourage you to feedback about your experiences and ideas to help us to research the areas that are important to you. Your treatment will not be affected in any way should you not wish to take part.
RADIOTHERAPY STAFF
CLINICAL ONCOLOGIST/REGISTRAR/CONSULTANT THERAPEUTIC RADIOGRPHERS
They are experts in radiotherapy and will be managing your treatment. They will take the responsibility for deciding what dose and how many treatments will be best for you; they will oversee the planning of your treatment. You may see them or a member of their team at your initial planning appointment and you may see them during your treatment.
THERAPEUTIC RADIOGRAPHERS
Therapeutic radiographers of any gender give radiotherapy, they are specialist healthcare professionals who are trained to plan and deliver radiotherapy treatment and to use the specialist equipment deliver radiotherapy. You will usually see the same team of therapeutic radiographers and they will assist you with any questions or problems or refer you to a more appropriate person.
RADIOTHERAPY SUPPORT TEAM
The team consists of Radiotherapy Nurses, Therapeutic Radiographers and Clinical Support Workers (CSW’s), based within the Radiotherapy Department where they actively support and advise patients receiving radiotherapy treatment. They offer advice to patients and their families/carers and are able to make appropriate referrals.
PHYSICISTS, PLANNING DOSIMETRISTS AND MACHINE TECHNICIANS
Medical physicists are specialist scientists who have a key role in the individual planning of your treatment, along with the planning dosimetrists. They may also have an input into the set-up of your treatment. They work together with the machine technicians to ensure that the machines are reliable and working accurately.
STUDENTS/THERAPEUTIC RADIOGRAPHER APPRENTICES
At some point during your treatment, you may encounter student radiographers/therapeutic radiographer apprentices. Everything they do is fully supervised. If you would prefer our students not to be present during the planning and treatment, please let a member of staff know when you attend for your initial planning appointment.
OTHER MEMBERS OF STAFF
During your treatment course, you may meet our receptionists, dieticians, oncology health staff, patient services staff, porters, and volunteer workers. All are important members of your care team, working together to provide you with high quality healthcare.
CONTACTS
Here are contact details of useful organisations that provide information and support about cancer including radiotherapy treatments:
Cancer Psychological Service
Can help with achieving the best possible quality of life during and after your journey with cancer.
Offer emotional support and practical help.
Discuss any matters that are concerning you and your family.
For a call back from the drop in team call 01482 461060/461061 Monday- Friday between 8.00am and 4.00pm
Macmillan Cancer Support
Provide information from specialist nurses on all aspects of cancer and its treatment, and on the practical and emotional aspects of living with cancer.
You can drop into the Macmillan Cancer Information Centre at the Queen’s Centre or call them on (01482) 461154 Monday – Friday 9.00am – 5.00pm.
Alternatively, free phone the national help line: 0808 808 0000 Monday – Friday 9.00am – 8.00pm.
Online: http://www.macmillan.org.uk
Write to Macmillan Cancer Support, 89 Albert Embankment, London, SE1 7UQ
General advice and Consent
Consent to Treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation, which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
For radiotherapy, you will be given both verbal and written information and after having time to ask questions, you will be asked to sign a consent form to show you have received enough information and you understand it. The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid.
That means:
you must be able to give your consent
you must be given enough information to enable you to make a decision
you must be acting under your own free will and not, under the strong influence of another person.
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, your information will be shared between members of the healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health or social organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018, we are responsible for maintaining the confidentiality of any information we hold about you. For further information, visit Confidential Information about You
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.
This leaflet was produced by the Radiotherapy Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in June 2025 (3 years)
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.




