- Reference Number: HEY-983/2022
- Departments: Emergency Department, Paediatrics
- Last Updated: 14 January 2022
Introduction
This leaflet has been produced to give you general information about your child’s condition. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for your child.
What is viral induced wheeze?
Wheeze is a noise made in the chest, mostly when breathing out. In viral induced wheeze the chest becomes wheezy and feels tight when the child has a viral infection (a cough, cold or chest infection). The wheeze happens when the tubes carrying air to the lungs (airways) become irritated and inflamed by the virus, causing them to swell and narrow.
Viral induced wheeze is common, affecting nearly a third of all children, but is more likely if your child was born early, ever had bronchiolitis or is exposed to cigarette smoke.
Does this mean my child has asthma?
Viral wheeze causes similar symptoms to asthma, but is a different condition. Some children will go on to develop asthma as they get older. Children with asthma can get wheezy even if they do not have a cough or cold. They are often wheezy if they do lots of exercise. Children with asthma often have a family history of asthma, eczema or allergy.
What treatment will my child need?
A “reliever” inhaler such as Salbutamol (blue inhaler) may be prescribed to be given using a “spacer”. This medicine relaxes the airways in the chest and makes it easier to breathe. The inhalers are safe and effective, but can raise your child’s heart rate and sometimes make them feel shaky or given them a headache. This will not harm your child and will soon settle. Some children may be given Montelukast, a medicine to be taken daily to help relax the airways. Antibiotics are not useful against viruses, so are of no use in viral induced wheeze. The illness will get better by itself once it has run its course. Similarly, steroids are not usually helpful in viral induced wheeze.
Sometimes if children are very breathless a nebuliser may be used, to give the medicine as a mist from a mask. If children need nebulisers or oxygen, or are having trouble feeding, they may be admitted to hospital. Medications may be given intravenously (into a vein) if a child is very breathless.
How can I care for my child at home?
- Give them plenty of rest and avoid stressful situations
- If they become warm and have a temperature, give paracetamol or ibuprofen, if your child can take it (always read the label)
- Give them the reliever blue inhaler as directed on this leaflet
- Encourage plenty of fluids and let them eat if they feel up to it
- Keep them off school or nursery until you feel they have recovered
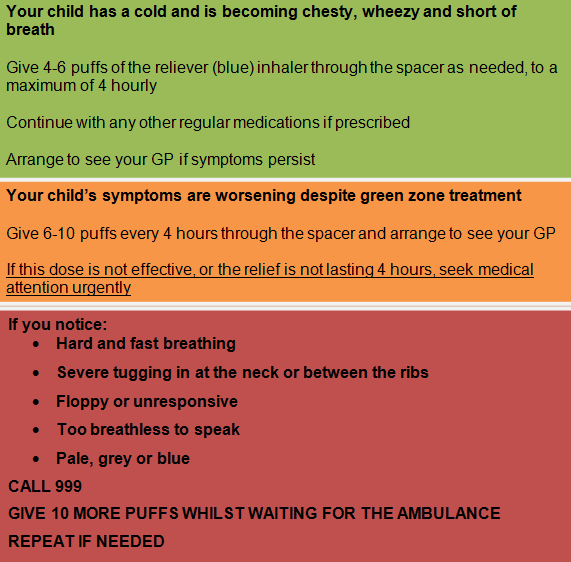
Treatment Plan