- Reference Number: HEY-982/2022
- Departments: Emergency Department, Paediatrics
- Last Updated: 14 January 2022
Introduction
This leaflet has been produced to give you general information about your child’s condition. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
Your child’s inhaler
Your child has been given an inhaler to help with their breathing.
“Reliever” inhalers (usually blue, Salbutamol) help to relax the airways and so relieve breathlessness.
“Preventer” inhalers (often brown) help to prevent the airways becoming narrowed.
Using a “spacer” (or Aerochamber) helps to get more of the medicine into your child’s airways.
It is important that you give the medicine as prescribed.
If anything in this leaflet is unclear, please ask your doctor, nurse or pharmacist.
How to use the inhaler and spacer
- Wash your hands.
- Shake the inhaler well and remove the cap.
- Attach the inhaler onto the end of the spacer.
- Place the mask over the child’s mouth and nose, or if using a mouthpiece, place it in their mouth
- Ensure there is a good seal around the mask or mouthpiece. You should see movement in the valve on the yellow Aerochamber or spacer as your child breathes.
- Press the inhaler once and allow your child to take 5 slow breaths in and out of the spacer. If your child is breathing very fast, leave it on for 10-15 seconds.
- Remove the spacer mask from your child’s face or the mouthpiece from their mouth. Shake the spacer and attached inhaler, to get it ready for the next dose.
- Repeat the process until your child has had the prescribed amount of puffs.
- Remember to shake the inhaler between each puff, otherwise your child will not get all of the medicine.
- Only put one puff of medicine into the spacer at a time. Anymore and the droplets of spray stick together and coat the sides of the spacer before your child can breathe it in.
Tips
- If possible, sit your child upright, as this will help them to breathe in the inhaler medicine.
- They may prefer to sit on your lap.
- It may help to breathe with your child so they can copy you.
- You may want to make it into a game, or use a small reward to encourage them.
- You could decorate the outside of the spacer with stickers.
- You could pretend to use the spacer on a doll or teddy too.
Cleaning the spacer
This only needs to be done once a month and the spacer should be replaced once a year. It does not matter if the clear plastic tube starts to look cloudy.
Remove the inhaler port (where the inhaler fits in) and soak both parts of the spacer and mask or mouthpiece in warm soapy water for 15 minutes. Rinse with hot tap water and leave to air dry in an upright position. Do not put any parts of the spacer in the dishwasher.
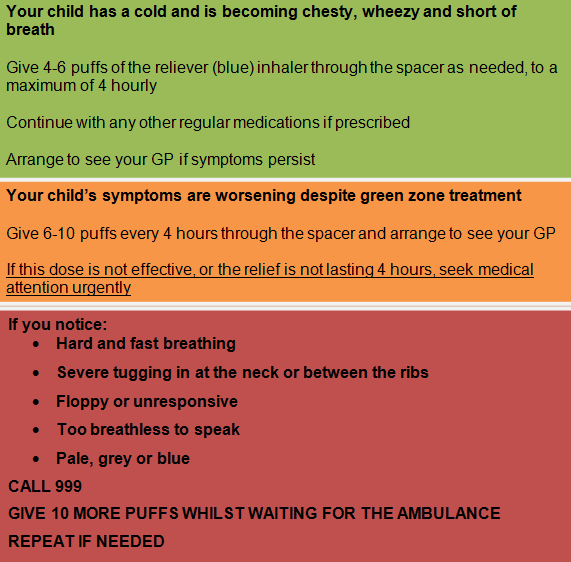
If your child is becoming more breathless: