- Reference Number: HEY1163/2023
- Departments: Pain Medicine, Psychology Services
- Last Updated: 1 November 2023
Introduction
This service works specifically with people living with chronic pain to help them to manage pain related issues. The clinical psychologists within Pain Psychology work alongside the wider Pain Management team. A referral to see a clinical psychologist in the team does not mean that the team believe your pain to be ‘fake’ or ‘all in your head’. As a service, we acknowledge that your pain is real and the clinical psychologist aims to work with the psychological and emotional impact that pain has on your life and to improve your overall wellbeing.
It can often be difficult to diagnose or effectively treat chronic pain with medical intervention and many individuals reach a point where further investigations and treatments are no longer helpful. As there are connections between your mind and body, it is important to understand and work with the processes that your brain is responsible for such as thoughts, feelings and behaviours to find a way to move forward with managing your pain. The clinical psychology team aim to help you live life more fully and meaningfully even with the presence of persistent pain.
The aim of pain psychology
Common reactions to the experience of chronic pain such as feeling frustrated, upset, low in mood, worried or anxious are normal and understandable. However, these reactions can also contribute further to the problem and make pain harder to cope with as the ‘pain cycle’ can keep people feeling ‘stuck’ in the struggle. The aim of individual psychology appointments is to help you to understand the difficulties that pain can bring to your life and to develop strategies which help to manage your pain now and in the future.
You and your clinical psychologist will agree the number of sessions you expect to have to complete your focused goals in your first session. Throughout the work you complete together, it will be expected that you attend and engage in each of the sessions. An important part of psychological work, and where the majority of positive and lasting change happens, is when you try out new ideas and skills between sessions following the conversations with your clinical psychologist. It is important that these skills are practised in your day-to-day life, so that you can build motivation and confidence to continue implementing them yourself once your sessions come to an end. The aim is to help you to become your own pain psychologist – you are the expert on you.
Clinical psychologists are trained to use a combination of evidence-based psychological approaches to meet your needs, including Cognitive Behavioural Therapy (CBT), Acceptance and Commitment Therapy (ACT), Compassion Focussed Therapy (CFT) and Eye Movement Desensitisation and Reprocessing (EMDR). The clinical psychologist will discuss these different approaches with you to come to a shared understanding of what might be most beneficial.
Why might pain psychology be for me?
Clinical psychologists for chronic pain can help with a variety of problems, including but not exclusive to:
- Improving understanding of chronic pain and how to manage it by making breaks in the ‘pain cycle’
- Developing strategies to cope with stress and difficult emotions such as fear, frustration and sadness that are caused by, or contribute towards pain
- Adjusting to loss of role(s) due to chronic pain
- Exploring difficulties within work, home life and relationships due to the impact of chronic pain
- Exploring how historical and current life factors may be influencing your coping with pain
- Managing the reduction of pain medication if this is advised by the Specialist Pain Team
- Improving mobility and working together with the physiotherapist
- Helping you to lead a life that is as normal as possible; identifying what is important and helping you to engage with this at a manageable pace.
Who, when and where?
- You will see one of the clinical psychologists working within Pain Psychology and usually this will be the same person at each appointment. From time to time, there may be clinical psychologists in training with the service who are also capable of carrying out the identified psychological work, under the supervision of a qualified clinical psychologist.
- Normally you will have 6–10 sessions with the clinical psychologist, and each session can be up to an hour long. The course of sessions may be shorter or longer depending on your individual needs. These sessions are usually face-to-face and will generally occur on a fortnightly basis on weekdays at the Queen’s Centre at Castle Hill Hospital or occasionally at the East Riding Community Hospital in Beverley. It is recognised that it can be difficult for some people to attend regular in-person appointments at the hospital and this can be discussed further with the psychologist.
- You may decide at any point during your psychological work that you do not wish to continue. This is something that should be discussed with your clinical psychologist but it is ultimately your decision and this decision would be supported.
What happens when I am referred?
Clinical psychologists work closely with other professionals within what is called a Multi-Disciplinary Team (MDT). The other pain professionals involved in your care might include consultants, pain nurses and a physiotherapist. We aim to provide a holistic or ‘whole body’ approach to your care and there is good evidence that medical care is more effective when you are able to be supported and work together with a wider team.
Any professional involved in your pain management care and connected to the hospital can refer to the psychology service. A member of the Pain Management MDT will first identify a potential need for the role of psychology as part of your pain management plan. You must have consented to this referral before it is accepted. It is your decision if you wish the referral to be made and you are welcome to ask your referring professional any questions about the service which might help you to make an informed decision about psychological support.
After the referral is received, one of the clinical psychologists within the team will then arrange a convenient time to complete an assessment with you to discuss whether psychological input focused around pain is likely to benefit you. They will ask you questions about how pain has impacted on your life and explore other background factors such as social history which may help to further understand your current situation. You may wish to bring a family member, friend or carer with you to the appointment. It is up to you if you want them to come into the appointment with you but it can sometimes be helpful to hear things from another person’s perspective, as well as having some time to discuss things one-to-one with the psychologist. We do ask that you do not bring any children with you to the appointments as this may limit your ability to speak freely. We also normally ask for subsequent sessions that you attend alone as it is important that a safe and private space is provided for you to discuss whatever may be troubling you, however this can also be discussed further with your psychologist.
Following the assessment, the clinical psychologist may identify that a short-term course of individual psychological therapy may be beneficial and further appointments will be arranged. Alternatively, it might be identified that a different service would better suit your needs and the psychologist can offer support with further referrals and signposting. For example, if the main source of distress is not related to pain but other mental health factors, then a referral to mental health services would be more appropriate. The psychologist can help you get the right support for your own individual circumstances.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Department of Psychological Services on tel no: 01482 461 060/061
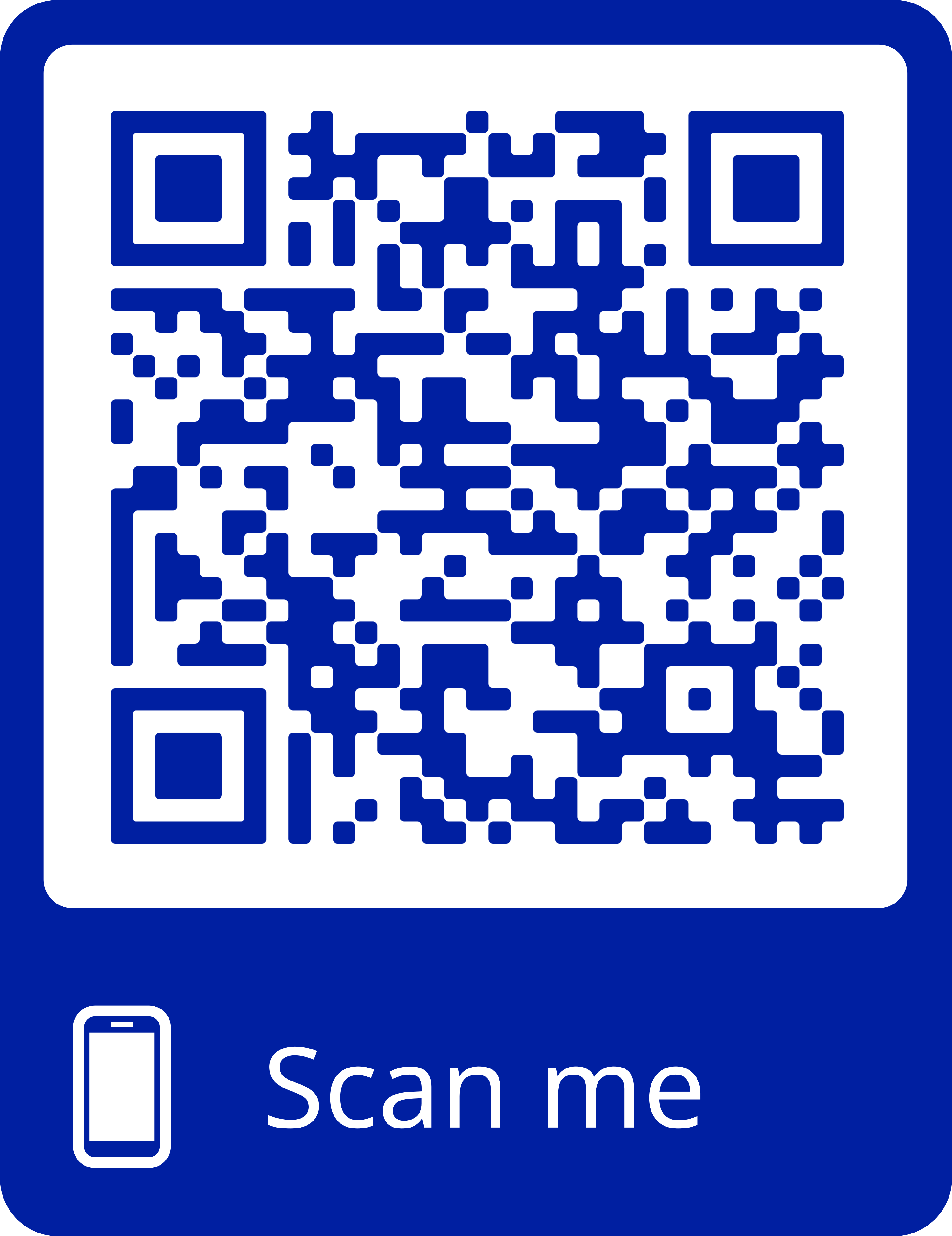
Please note that this service cannot provide urgent mental health support. If you require crisis support, we urge you to contact the 24/7 Mental Health Crisis Team which can be found by searching for your postcode on the following website link: https://www.nhs.uk/service-search/mental-health/find-an-urgent-mental-health-helpline. In Hull, the contact telephone number is: 0800 138 0990. If you are in imminent danger, phone 999.