- Reference Number: HEY-248/2021
- Departments: Orthopaedics
- Last Updated: 19 January 2021
Introduction
This leaflet has been produced to give you general information about your injury. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a knee soft tissue injury?
The knee is a complex joint which is designed to withstand large stresses. Its stability relies mainly on:
- Ligaments – which are strong bands of tissue that connect one bone to another and help hold the knee joint together.
- Meniscus – This is the cartilage tissue which acts as a shock absorber in the knee joint.
- Muscles – which surround the knee joint.
Any one or a combination of these structures can be injured.
What are the symptoms?
Symptoms can vary depending on the structure that is injured. Acute knee injuries may cause:
- Pain, swelling and / or bruising.
- Locking (an inability to straighten the knee).
- Giving way.
What if I need pain relief?
To manage your pain it is advised that you regularly take simple pain relief, which can be bought over the counter from a pharmacist. If you have allergies or conditions which prevent the use of pain relieving or anti-inflammatory medication, please seek advice from your doctor or a pharmacist.
What should I do in the first 72 hours after the injury?
The most important initial treatment is aimed at controlling the pain and swelling by following the principles of RICE:
R – Rest
Complete rest is not advisable but it is important that you prevent putting the knee under strain in the very early stages of healing. If necessary you will be given crutches to help you take some weight off the injured knee.
I – Ice
Ice will help reduce the pain in your knee and so should be applied for 10-15 minutes. This will help to reduce the swelling.
There are many different ways in which ice can be applied however it is believed crushed ice, in the form of frozen peas for example, is the most effective. Whichever method you choose it is important that you wrap the ice in a damp towel, in order to prevent it from ‘burning’ the skin.
Please note:
Only use an ice pack on areas that have normal skin sensation i.e. where you can feel hot and cold.
Do not apply over an open wound.
Do not apply an ice pack to an area that has poor circulation.
When you apply ice to your skin, check the skin every 5 minutes and discontinue its use if:
- the area becomes white, blue or blotchy.
- the area becomes excessively painful, numb or tingles.
C – Compression
You may have been given a tubigrip to wear to help control your swelling. It is important this is removed if you develop any signs of poor circulation such as tingling, numbness, blueness of the skin of the foot and increasing pain. The tubigrip should be removed when you go to bed at night as when you are asleep you cannot monitor these symptoms.
E – Elevation
 |
The ankle should be elevated above the level of the heart as much as possible, as this will reduce and prevent swelling in your knee. |
What not to do
Consuming alcohol, massaging the injured area and applying heat can all be detrimental in the early stages of healing and therefore should be avoided. It is important to note that smoking may also delay the healing process.
Rehabilitation and recovery
If you follow this basic advice your injury should take around 6 weeks to heal. However, everyone recovers from injuries at different rates and it is dependent on the severity of the injury, the soft tissue that was involved and the presence of any other medical problems.
After 72 hours it is important you try to practice the following exercises which will help you to regain full function, flexibility and strength. These will also reduce the risk of the injury occurring again.
1. Find a friction free surface, for example a wooden floor or a tea tray placed on your bed, so that your foot can slide easily.
 |
Sit down and stretch your legs straight out in front of you. Now slide your foot up towards your bottom by bending your knee.
You may want to wrap a scarf around your heel so that you can assist by pulling with your hand to bend your knee further. |
2. Sit on the floor or bed with your legs straight in front of you.
 |
Tighten your thigh muscle by pushing the back of the knee downwards and raising your heel slightly.
Hold for 5 seconds. |
Each exercise should be repeated 10 times, 3 – 4 times per day.
As the knee improves you will find that you are able to stand and walk for longer. At this stage you should add in the exercises below.
1. Lean against a wall with your feet hip width apart.
 |
Now bend both knees so that you slide down the wall.
When you feel that your heels begin to lift off the floor, stop, hold 5 seconds and then return to the starting position. |
2. Stand facing a wall and hold on for support.
 |
Keep your knees together; lift the heel of the injured leg up behind you towards your bottom.
Hold for 5 seconds and gently lower. |
3. Stand facing a step and hold on to a firm support if required.
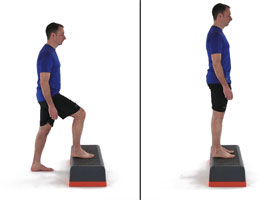 |
Place the foot of the injured leg on the step and step up
Now place the foot of the uninjured leg on the floor and step down. |
4. Stand on your injured leg and balance. To begin with you may need to hold on to something solid to prevent you from falling over.
 |
As you improve try doing functional activities such as washing the dishes or cleaning your teeth while you are standing on the one leg.
Try to hold your balance for up to 30 seconds. |
Each exercise should be repeated 10 times, 3 times per day.
All photos with kind permission of ©Physiotec™
When can I return to normal activities?
If you participate in an active hobby then it is advisable that you do not return to this until you have full strength, full range of movement and you can walk briskly, run and turn without experiencing pain and swelling.
If you play a sport, practice specific activities like dribbling or jumping to prepare the knee and build this up gradually before returning to full training sessions and competition.
Do I require further treatment?
You may be advised that you require physiotherapy following this type of injury, unless your symptoms are minimal on your initial appointment. Your physiotherapy could be at a variety of locations in the Hull and East Riding area.
You can self-refer to physiotherapy by contacting the following number depending on the location of your doctor:
- Hull GP patients self-refer to Healthshare: (01482) 300003
- East Riding GP patients self-refer to East Riding Physiodirect (01377) 208300 or self-refer online at chcpmsk.org.uk
On occasions the clinician may wish to refer you to the physiotherapy team within the hospital trust. If this is the case they will advise you of this and you should receive an appointment at Hull Royal or Castle Hill Hospitals within 5 to 7 days of your attendance at the Emergency Department. If you have received no contact within this time please call the physiotherapy admin team on (01482) 674880.
When to seek further help
If 10 days following your injury you are unable to weight bear and the knee remains painful and swollen, despite following the advice in this leaflet, please contact the physiotherapy team that you were advised to contact at your Emergency Care attendance.
Please be aware it is very important that you see your doctor immediately if, after following advice in this leaflet you notice that the calf becomes increasingly tender, red and that it is tender and hot to touch.

