- Reference Number: HEY1231/2021
- Departments: Orthopaedics
- Last Updated: 18 May 2021
Introduction
You have undergone the placement of an external fixator and are being cared for by the Limb Reconstruction service. This information sheet aims to help you, your family and friends to recognise and understand the process of psychological recovery and common emotional reactions to living with an external fixator. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
Preparing for surgery, undergoing the placement of an external fixator and living with the frame can all lead to a number of normal and common psychological reactions. This can be as part of the process of adjusting to the function and appearance of the frame as well as processing the circumstances that led to your limb reconstruction journey.
Common emotional and physiological responses include:
- Hypervigilance: feeling jumpy, panicky, or sensitive to particular sensations or sounds more than normal. This happens as your body is in a heightened state of arousal, paying more attention to your surroundings in an attempt to feel safe.
- Re-experiencing: You may experience dreams or flashbacks; in some cases, you may see/hear/feel/smell an event again. It may feel very real at the time, like it is happening in the present moment, and these may come with no warning or seemingly no conscious control, making these experiences unpleasant and distressing at the time.
- Thoughts: You may find you become stuck on things you wouldn’t normally think or experiencing “what if…” thoughts. Our minds can feel over active as we try to process the distressing events we have experienced.
- Changes in mood: You may find your emotions are more changeable or rawer than usual or that you experience lots of different emotions in a short space of time. Some people feel numb or find it difficult to work out how they feel.
- Avoidance: Sometimes people wish to avoid reminders of the event. They may prefer not to think or talk about it, want to be alone, or avoid places or situations that cause distress.
- Depersonalisation: It may feel like you are disconnected from your difficult experiences. You may feel numb or as though it did not happen to you, perhaps dream-like or as though you watched it happen in a film. This depersonalisation and numb feeling may be a way of slowly and gradually opening up and feeling the distress of your journey or a particular event.
- Physical symptoms: As your body is processing your injuries and how they were sustained, you may notice physical symptoms such as palpitations (heart thumping), changes to breathing, poor sleep, nausea, headaches, poor concentration, tension or pain.
How long might this last?
In most cases these psychological reactions are short-term and will pass after a few days or weeks as your body adjusts to the external fixator and recovers. However, sometimes these reactions can last longer depending on your circumstances and emotional response. Factors such as length of your hospital stay, duration of wearing the frame as well as a number of psychosocial factors could impact on your reaction. This is also normal in the early stages of recovery.
Delayed or longer-term stress reaction
Sometimes, the common responses identified above can last for longer. This is still quite usual, but you may want to seek further help if you find they are persisting for more than four weeks or if feel you need support in managing the intensity of these symptoms in the early weeks after discharge home.
You may find that your emotions and stress reactions begin to feel manageable whilst in hospital, but symptoms may re-remerge or become more overwhelming once you leave. This can be due to the changes you are experiencing that can make you feel less safe and certain and likely will have new challenges to adjust to (e.g. returning to normal routines). Emotional difficulties at this stage are still resolvable, but can benefit from psychological input.
What can I do to help?
- Remember your reaction is normal.
- Allow yourself the time to process and accept what has happened. It is similar to other times of loss, you may need to grieve for the changes in your life and take time to heal.
- Talk to people about your experiences; simply sharing your feelings can help you process them and help your body calm. You may find it helpful in time to find out more about what has happened.
- Rest and eat well. Your limb reconstruction journey will been a physically and emotionally exhausting experience, and you will benefit from taking time to rest and let your body get sufficient sleep, and maintain energy by having a good diet (this may be managed for you by the hospital staff).
- Think about some activities that you usually enjoy and return to these when possible. If this is not possible perhaps you could try something new or plan these positive events for your recovery. Some people also find having a structure or routine around them helpful.
- Allow yourself to feel this range of emotions and think it over. Do not worry about crying or if you are struggling to make sense of it all to begin with.
- Seek help and ask for support, either from the staff here or from your doctor if you are worried about your symptoms and experiences.
- When we feel high moments of distress try grounding yourself to the present moment. A simple technique for doing this is the 54321 method: thinking of 5 things you can see, 4 things you can hear, 3 things you can feel, 2 things you can smell, and take 1 deep breath.
- Welcome relaxation, try spending 2 minutes taking some slow deep breaths, and try visualising somewhere that makes you feel calm and comfortable. This helps our bodies feel safe and relaxed so that our energy can go towards healing our physical injuries.
Things that are best avoided
- Try not to distract yourself from thinking about it, for example by being very active, taking on too much or going back to work very quickly. This again may prevent you from processing what has happened; instead take some time to help you come to terms with any changes.
- Avoid alcohol and manage medication well. Other ways people may try to distract themselves is by using alcohol or medication to “numb the pain”. Your brain needs to process your experiences, and a high level of distraction or avoidance can disrupt this process.
- Do not bottle up your emotions. We are sometimes taught to manage our emotions and not “let it all out”, but emotions are a physiological natural response to circumstances around you. Allowing ourselves to feel and express them can help give us a sense of relief.
Accessing support after you leave hospital
Your local Improving Access to Psychological Therapies (IAPT) NHS Service can continue to help you should you feel you would benefit from some emotional wellbeing support. These services offer support to people with common mental health difficulties, such as anxiety, depression, stress and some types of trauma.
The support they provide ranges from guidance on self-help material, psycho-educational groups, and more individual one-to-one sessions either over the phone or in person.
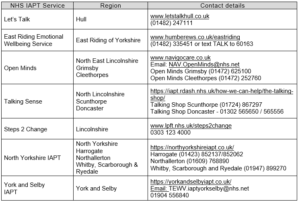
You can gain access to this support through your doctor, or you can easily refer yourself by phoning them directly. To find out how, you can search online for your local service. Below are the contact details for some of the local services:
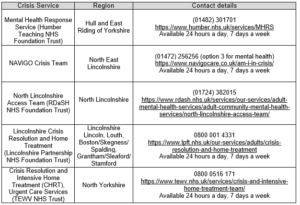
Urgent Mental Health Support If you require urgent mental health support to keep yourself or others safe, you can access this by calling the following services in your local area, or by calling 999 or attending your nearest Emergency department.
Additional Helpful Numbers
- Mind Info line- 0300 1233393
- Samaritans- 116 123 (free at anytime, from any phone)
- HEADWAY brain injury association 0808 800 2244 or 07395 571398 for Hull & East Riding’s branch (headway.org.uk)
- PAUL for Brain Recovery – 01482 620229 (paulforbrainrecovery.co.uk)
- Cruse Bereavement – 01482 565565 / 0808 808 1677 (cruse.org.uk)
- Spinal Injuries Association – 0800 980 0501 (spinal.co.uk)
- Hull DAP (Domestic Violence) – 01482 318759 (hulldap.co.uk)
- DVAP (East Riding Domestic Violence support) – 01482 396330
- Citizens Advice – 0344 411 1444 (e-advice@hull-eastridingcab.org.uk)
- CGL Renew Hull (Drug and Alcohol service) – 01482 620013 (hull@cgl.org.uk)
For additional information about services in your locality, please contact your doctor.
