- Reference Number: HEY-854/2019
- Departments: Nutrition Support
- Last Updated: 15 July 2019
You can translate this leaflet by selecting a language from the dropdown menu:
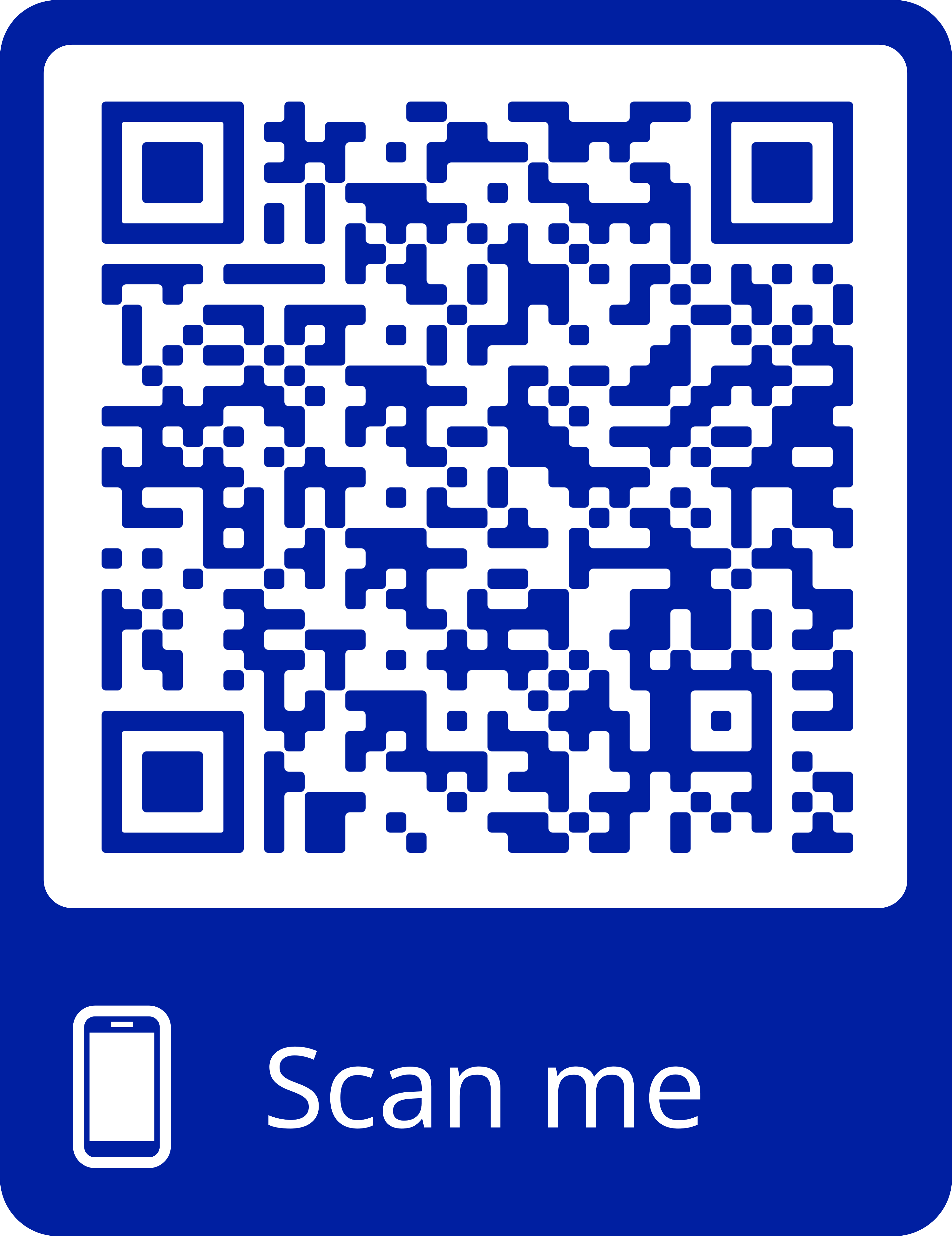
This leaflet has been produced by the Hull University Teaching Hospitals NHS Trust and is available as a download:
Download the “Jejunostomy (JEJ) Feeding Tube – Passport” leaflet