- Reference Number: HEY130-2024
- Departments: Maternity Services
- Last Updated: 30 April 2024
Introduction
This leaflet has been produced to give you general information about the effects a raised body mass index (BMI) can have on your pregnancy and in labour. It will explain what you can do to reduce your risk and improve your health by having a healthy lifestyle.
Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your midwife or doctor, but can act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is a raised BMI?
Your BMI is calculated by dividing your weight (in kilograms) by your height (in metres) squared.
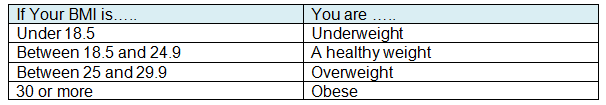
Early in pregnancy you will have had your BMI measured. If it is 30 or more, you have a higher risk of complications for you and your baby.
How does this affect my pregnancy?
Being overweight increases the risk of:
- High blood pressure and pre-eclampsia.
- Developing diabetes.
- Developing a blood clot (thrombosis) in your legs or lungs
- Early miscarriage.
- Having a baby who is too big (macrosomia)
- Labour being induced
How does this affect my labour?
Being overweight:
- Increases the chance of labour progressing slowly resulting in a longer labour
- Makes it more likely that assistance will be required to help deliver the baby, for example; ventouse (a suction cap attached to baby’s head) forceps or emergency caesarean delivery.
- Increases the risk of infection
- Increases the risk of heavy bleeding
- Increases the risk of the shoulders getting stuck at the birth (shoulder dystocia)
- Increases the risk of stillbirth
If you decide to have an epidural for pain relief, it might be difficult and take longer to insert.
How does this affect me after the baby is born?
Baby is also more likely to be overweight and develop diabetes in later life. You may have an increased risk of developing an infection.
What can I do to help?
Simple things really can make all the difference.
- Watch the portion size of your meals and snacks and how often you eat
- Do not ‘eat for two’
- Eat a low-fat diet
- Eat as little as possible of the following: fried food, drinks and sweets/biscuits high in added sugars, and other foods high in fat and sugar
- Eat fibre-rich foods such as oats, beans, lentils, grains, seeds, fruit and vegetables as well as wholegrain bread, brown rice and pasta
- Eat at least five portions of a variety of fruit and vegetables each day
- Choosing wholegrain where possible
- Make activities such as walking, cycling, swimming, low impact aerobics and gardening part of your daily life
- Take the stairs instead of the lift or go for a walk at lunchtime
- Do not sit for long periods like watching television or at a computer
Exercise will not harm you or your unborn baby but, if you are new to exercise you should begin with 15 minutes of continuous exercise, three times per week, increasing gradually to 30 minute sessions every day.
You can join groups for extra help and support:
- HEY Baby – Antenatal and parenting classes
- USMUMS – from aqua aerobics to Zumba
- HENRY – A great start for babies and young children
Helpful websites
Should you require further advice on the issues contained in this leaflet, please contact the Public Health Midwife on telephone number on tel: 01482 607838.

