- Reference Number: HEY640-2024
- Departments: Neurology and Neurosurgery, Physiotherapy
- Last Updated: 3 June 2024
 Introduction
Introduction
This leaflet has been produced to give you information about your spinal brace. Most of your questions should be answered by this leaflet. It is not meant to replace discussion between you and your physiotherapist or surgeon, but may act as a starting point for discussion.
Your consultant should have explained the reason for having to wear your spinal brace. This leaflet will concentrate on providing you with the information on the physiotherapy input you can expect and instructions for your spinal brace.
If after reading this leaflet, you require further explanation please discuss this with a member of the physiotherapy team.
What is a spinal brace and why do I need it?
A spinal brace is a device designed to limit movement of the spine. It is most commonly used to manage spinal fractures but can also be used for other reasons such as supporting your spine after surgery.
Limiting the movement of the spine through wearing a spinal brace helps the healing process. It may also help to prevent further injury or damage and can help to minimise discomfort.
Can there be complications with wearing a spinal brace?
Movement cannot be completely stopped within your spine and so occasionally a spinal brace may not be sufficient to manage your condition and you may require other treatments.
Wearing a spinal brace will cause some weakness of the muscles around your spine, as the spinal brace will essentially be doing some of the work of these muscles. However, when you no longer require your spinal brace you will be advised to gradually stop using it and you will be provided with an exercise program to strengthen your muscles again.
Applying your spinal brace
Use of the spinal brace could cause pressure leading to redness or, in extremely rare circumstances, breaking of the skin. Experienced physiotherapists will measure and fit you into the spinal brace to ensure it is not ill fitting. You will be instructed to remove your spinal brace daily when you lay down to sleep.
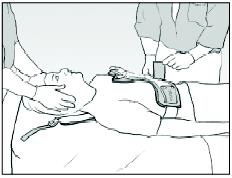
The physiotherapist will measure you and determine which spinal brace is most suitable for your size and shape. Initially your physiotherapist will fit your spinal brace while you are lying down. They will then give you instruction on the way in which the spinal brace should be applied and removed.
Spinal brace should be applied and removed in one of the following ways:
Your physiotherapist will let you know which option
Option 1 – Lying
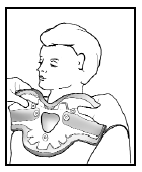
1. Roll onto your side.
2. Feed the fabric side strap under your body at waist level.
3. Roll back onto the brace ensuring the brace is centrally located.
 ® Aspen
® Aspen
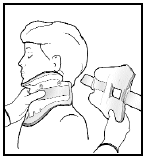
4. Attach the neck collar component as follows:
- Position the chin piece directly under your chin and push the sides of the front panel around your neck.


 Aspen®
Aspen®
 ® Aspen
® Aspen
- While holding the front of the collar attach the Velcro sides.
- Tighten neck collar enough to ensure that the back panel flexes to fit the back of your head.
5. Slide the buckles on the fabric side straps into position, onto the front panel of the brace.
 ® Aspen
® Aspen
Option 2 – Sitting
1. Position yourself on the edge of the bed (see next page for technique)
2. Attach the neck collar component as follows:
a. Position the chin piece directly under your chin and push the sides of the front panel around your neck.
 ® Aspen
® Aspen
b. While holding the front of the collar centre the back panel and attach the Velcro sides.
 ® Aspen
® Aspen
c. Tighten neck collar enough to ensure that the back-panel flexes to fit the back of your head.
3. Ensure the front of the brace is positioned centrally.
4. Slide the buckles on the fabric side straps into position, onto the front panel of the brace.
 ® Aspen
® Aspen
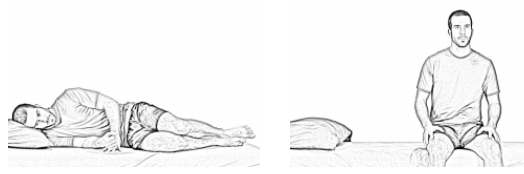
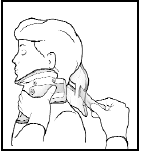
Moving from lying to sitting up
Roll onto your side and swing your legs over the edge of the bed, whilst pushing up with your arms (see following diagram). Please note the following:
- If you are sitting in order to apply your spinal brace please do so immediately after assuming the sitting position.
- If you are sitting in preparation to stand please sit for a moment before standing to ensure you do not become dizzy.
©Physiotec™
Removing your brace
To remove your brace return to the position it was applied in.
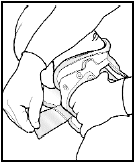
- Undo the straps around your waist by unfastening the buckles.
- Undo the Velcro on the neck collar section of the brace.
- Place it in a position where it can be easily reached for when you need to reapply.
Important information
Please note the following:
- A thin layer of clothing should be worn between you and the spinal brace to prevent rubbing or sores.
- The spinal brace should be TIGHT but COMFORTABLE
- If excessive sweating occurs, please remove the spinal brace and rest for short periods lying down – this is especially important if you have a wound from surgery.
- The spinal brace should be kept on at ALL times except when lying flat – you do not need to wear your brace in bed, unless you have been instructed otherwise by your physiotherapist or consultant. You may need to wear a collar overnight. If this is the case your physiotherapist will teach you how to apply and remove the collar.
- The spinal brace will only limit movement within your back, not remove it completely. It is important that you monitor your posture to prevent slouching, and avoid any bending, lifting or twisting.
- Bathing and showering are not permitted unless you are given special instruction from your consultant.
- If you feel you may need guidance with washing and dressing technique please discuss this with the occupational therapist on the ward prior to discharge.
- If you have any problems with the spinal brace please do not hesitate to contact the physiotherapy team on the number at the end of the leaflet.
Exercise
This exercise is aimed at maintaining strength in the muscles that support your back. It should be carried out three times a day, initially repeat each exercise just once and gradually build up over the period of a week to 10 repetitions of each exercise.
If you experience any increase in pain, cease from doing the exercise until the pain resolves, at which point you can recommence the exercise.
1.Breathing control in the lying position (Brace off). Put one hand on your upper chest and one hand on your abdomen just below your rib cage. Relax the shoulders and hands. As you breathe in, allow the abdomen to rise, and as you breathe out, allow the abdomen to flatten. There should be little or no movement in the chest. Try to slow your breathing down. Using this exercise often helps decrease muscle tension and relieves pain.
 ©Physiotec™
©Physiotec™
2. Lie on the back with both legs bent and feet together (Brace off)
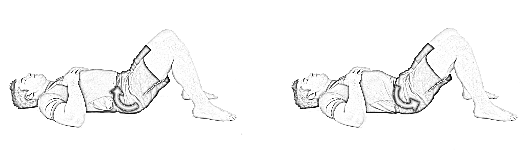 ©Physiotec™
©Physiotec™
Hollow your stomach and contract the abdominals to roll the tail bone off the floor. Do not push down excessively through your feet. Sustain the contraction using minimal effort for approximately 5 secs.
3.Complete this exercise in standing or in an upright sitting position (Brace on)
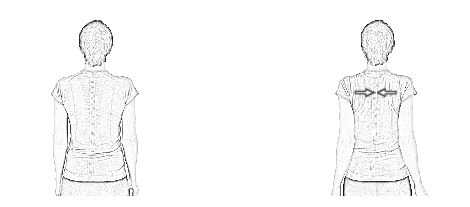 ©Physiotec™
©Physiotec™
Tuck your chin slightly and keep your spine tall. With your arms relaxed on your side, squeeze your shoulder blades together without shrugging them, hold for 5-10 seconds. Gently relax the position and repeat.
4. Complete this exercise in standing or in an upright sitting position (Brace on)
 ©Physiotec™
©Physiotec™
Stand with your arms relaxed on each side of your body. Make forward circles with your shoulders. Repeat in the opposite direction
5. Complete this exercise in standing or in an upright sitting position (Brace on)
 ©Physiotec™
©Physiotec™
Lift your arm up forwards letting your thumb lead.
You may also be provided with additional exercises to strengthen your back and legs if your physiotherapist deems this necessary.
General advice
Walking
Initially after your hospital admission your back may be sore as you move; this may increase over the first couple of days but will then improve. You should aim to walk short distances little and often to ensure your muscles do not stiffen up. Once you are home try to increase the distance you walk daily always paying attention to your posture.
It is important to strike a balance between periods of activity and inactivity. Inactivity can be just as harmful to your back as over activity.
Sitting
Whilst sitting out in a chair you should ensure a good upright posture. You should avoid standing still or sitting for prolonged periods as this will cause your back to stiffen and your posture to deteriorate.
Avoid sitting in soft low chairs as this will cause your back posture to become rounded even with the support of the spinal brace.
Lying
A good firm support is usually desirable; a mattress that is too soft will provide you with little support. You are free to move around in bed but you must ensure, where possible, that your position is not twisted (i.e. legs and body are aligned and pointing in the same direction).
Work
Returning to work will depend very much upon the individual and the type of work you do. It is important that you ask your surgeon when it is safe to return to work.
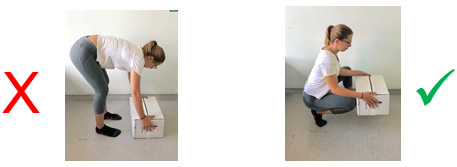
Lifting
Do not lift heavy objects and avoid holding items at arms length. Always use a correct lifting technique, bending at the knees and not at your back (see following diagram). Avoid bending, twisting or leaning movements as these will increase the strain on your back.
Discharge and follow up
Often patients manage by themselves straight away, sometimes family members/carers are taught how to help apply and remove the spinal brace.
You will also need to be able to sit comfortably in the spinal brace, walk short distances and be able to walk up and down a flight of stairs (if you have them at home).
You may be expected to attend for follow-up X-rays to monitor the healing process. If this is the case then you will be provided with dates and times for these appointments by your physiotherapist. Please attend X-ray first and then to see the physiotherapist. Please allow good time for these appointments as occasionally there can be delays.
When to stop wearing your spinal brace
The spinal brace is usually worn for a period of 8 weeks, to support your back and prevent movement around the fracture site, but this can alter depending on your healing rate and your consultant’s opinion.
After your final X-ray you will be told if your fracture has healed sufficiently for you to be able to remove the spinal brace. The physiotherapist will discuss this with you and give you further instruction at this point.
You will be advised to gradually reduce from your spinal brace to prevent sudden strain on your back and also to help to strengthen your spinal muscles slowly to minimise discomfort. Your physiotherapist will advise you on this, recommending you decrease the time spent in the spinal brace daily over 1 to 2 weeks.
You may feel stiff initially in the affected part of the spine when you start to reduce the length of time spent in the spinal brace, this is normal, and will improve as your activity levels increase. The physiotherapist will provide you with exercises to improve this, and also to build up the muscle strength in your spine. If required, you may also be referred for out-patient physiotherapy to further support your recovery.
Once out of the spinal brace, you should try to maintain a good upright posture. The spinal brace will have supported you up until this point and slumping will cause additional strain on your muscles. Heavy lifting should be avoided and return to activity should be controlled. If you have any specific activities you wish to return to please discuss this with your physiotherapist for advice.
Should you require further advice about the issues contained in this leaflet, please do not hesitate to contact the Hull Royal Infirmary Physiotherapy Department on tel: 01482 674539 or Ward 4 Hull Royal Infirmary on tel: 01482 675004