- Reference Number: HEY1213/2021
- Departments: Cardiology
- Last Updated: 28 February 2021
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
The leaflet contains important advice about your discharge from hospital after your cardiac procedure, whether you have had a coronary angiogram or angioplasty. It contains information about what to do when you get home and how to maintain a healthy lifestyle.
- Discharge summary
- Medication
- Follow-up
- What to do when you get home
- What to do if you get chest pain
- Driving
- Return to work
- Support from cardiac rehabilitation
- How you contact us
Discharge summary
The procedure you had was ………………………………………………………………………………………………….
The results of your procedure were……………………………………………..…………………………………………..
The Consultant who performed your procedure was………………………………………………………..…………….
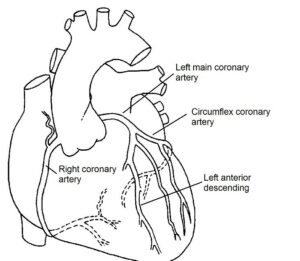
Coronary arteries
Medication
Your medication will be explained to you before you go home.
If you have had an angioplasty
You have had an angioplasty procedure because of an important narrowing within one or more of the arteries of your heart. The procedure was done to improve the blood supply to the heart. It involved stretching the narrowed area with a small balloon and, usually, a small metal scaffold device (stent) is left inside to keep the blood vessel open. After you go home following an angioplasty procedure there is a small risk of problems developing within the treated area so it is important that you read the following information.
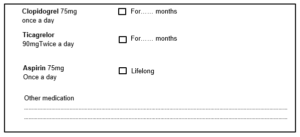
Blood clots: In approximately 1 in every 100 patients, the stent may suddenly block off due to a blood clot developing inside it (called a stent thrombosis). To reduce the chance of this happening, it is very important that you take 2 types of tablet to reduce the stickiness of the blood. One of these is Aspirin, which most people remain on for life. The other is called Clopidogrel or Ticagrelor and is usually needed for between 1 month and 1 year depending on the type of stent you have had – your doctor or nurse will tell you how long.
Sudden blockage of the stent due to a blood clot can cause sudden severe chest pain and can lead to heart attack or death. Most, but not all, of these clots occur within the first 7 days after the angioplasty so it is very important to call for emergency help (dial 999) if you get chest pain after the angioplasty.
Repeat narrowing: After the angioplasty has been performed, the same area may become narrowed again because of scar tissue. This is a process called restenosis, and usually occurs during the first 6 months after the procedure. If a lot of scar tissue develops then symptoms such as angina may come back and further treatment will be needed in around 1 in every 10 patients.
For most people this will be with another angioplasty procedure, though a few patients are advised that they should consider undergoing bypass surgery. If you are concerned that you are having symptoms then please see your doctor. Side effects
It is normal to experience increased bruising whilst on clopidogrel or ticagrelor, but please speak to your doctor if you are concerned or notice any unexpected bleeding or blood in your faeces or urine.
You should take the following medications, as well as any other regular medications you have been described by your doctor.
Anticoagulant medication
If you were previously taking anti-coagulant medication, such as warfarin, apixaban, Rivaroxaban, Dabigatran or Edoxaban, you will be advised when to restart before you are discharged.
Follow-up
After your discharge from hospital, we will send an electronic discharge to your doctor explaining your outcome and planned treatment, including any medication changes. It is important that we monitor your recovery after you have had an angioplasty, especially if you have any problems. In the next few months or years, we may contact you by telephone to see how you are getting on. Please keep us informed of any changes to your contact details. If you DO NOT want us to contact you please let the nurse or doctor know before you go home.
What to do when you get home and wound care
Your procedure will most likely have been performed from either the blood vessel in your wrist or at the top of your leg and it is common to be a bit bruised afterwards. If this is uncomfortable then take pain relief medication such as paracetamol. Do not take pain relief medication that contains aspirin, although you should take your prescribed aspirin in the usual way.
After your procedure you should rest the limb which has the insertion site (wound). The dressing should be kept on for 48 hours after the procedure after which it may be removed and you can take a shower as usual. It is advisable not to use a bath for a further two days and avoid putting talc or cream directly onto the puncture site.
Avoid heavy lifting or strenuous activity for 7 days after the procedure.
A lump may develop around your wound site. If it is the size of a pea then do not worry – this is just the scar. If, however, a large lump develops, which is bigger than a 10 pence coin or the site starts to bleed You must seek immediate medical advice. If the bleeding is from the groin you should then lie down and apply pressure. If it is from the wrist you should apply pressure and elevate the arm.
You should also seek advice from your doctor if you experience numbness, coldness or pain in the affected leg or arm.
It is important to remember that chest pain is not always the heart. However, any symptoms of chest discomfort should be taken seriously and the following steps taken:
- Stop what you are doing, sit down, rest, and try to relax.
- If you have a Glyceryl Trinitrate (GTN) spray, take 1-2 puffs under the tongue and wait for 5 minutes. Repeat if necessary (a total of 4 puffs in 10 minutes).
- If, despite this, the pain has not gone, or if you also have palpitations or feel sick, breathless or dizzy, then DIAL 999 FOR AN AMBULANCE.
Driving following elective or planned procedure
The DVLA make the following recommendations regarding driving:
- After an angiogram: do not drive for 3 days.
- After a planned angioplasty: do not drive for 1 week.
- If you have had a heart attack, a return to driving depends on how well the heart muscle is pumping. If the muscle pump has been weakened from the heart attack, driving should be delayed for 4 weeks. If no major damage has been done to the pump then you may be eligible to drive after 1 week. Your doctor will advise you.
If you hold a group 2 licence (LGV / PCV) then you will need to inform the DVLA of your condition and are not able to drive this type of vehicle for at least 6 weeks. (You may drive a car as per the guidelines listed above). You may need additional tests to fulfil the DVLA requirements for a group 2 licence.
You should discuss your individual circumstances with your doctor or nurse.
Travelling by Aircraft
Although it is generally not recommended to take a long haul flight shortly after an angiogram or angioplasty procedure, most people who are otherwise well, should be fine to fly. The UK Civil Aviation Authority advises all passengers to discuss their individual circumstance with their doctor. The general guidance regarding fitness to fly is as follows:
- After an angiogram or routine angioplasty, you may be able to fly after 2 days.
- After an uncomplicated heart attack, you may be able to fly after 3 – 10 days.
- After a more significant or complicated heart attack, delay flying for 4 – 6 weeks.
Please note that it is not recommended to travel outside the UK without medical insurance. You should inform your insurance company of your heart condition and should be aware that many medical insurance companies will not provide insurance within 1 month of an angioplasty procedure.
Returning to work
When you can return to work will depend on what you do for a job. General guidance is 3 days after an angiogram, and after 1 week following an angioplasty. If you have a heart attack then you will likely need 4-6 weeks off work. Please speak to your nurse or doctor about when you may return to work before you leave the ward.
Support from Cardiac rehabilitation services
Patients diagnosed with heart disease following an angiogram, patients who have had an angioplasty and patients who have had a heart attack will be referred to the Cardiac Rehabilitation Service. Cardiac rehabilitation is a tailored treatment and prevention programme, delivered by a team of healthcare professionals, which helps improve the health and wellbeing of people who have heart problems. It is important to take part in Cardiac Rehab as it can support you to improve your heart health. Your nurse will refer you to the community Cardiac Rehabilitation team who will contact you at home following discharge.
Lifestyle changes and prevention of future symptoms (secondary prevention)
If you have been told that you have some disease in your arteries then there are many things that you can do to improve the situation.
Coronary artery disease is one of the most common causes of death in the UK. By making some important lifestyle changes, you will help to reduce your risk of cardiac problems in the future.
The advice is relevant to everyone, not just people with disease in their arteries. By following it, you can maintain a healthy lifestyle. If you would like further information on any lifestyle issues, please ask your nurse or help yourself to the health education leaflets displayed.
Alternatively The British Heart Foundation produces a number of patient leaflets which can be ordered from them or downloaded from their website: www.bhf.org.uk
The risk factors are:
- Smoking
- Eating an unhealthy diet
- Family history of heart disease
- High cholesterol levels
- If you have diabetes
- How much exercise you take
- High blood pressure
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
How to contact us
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Cardiology Department on telephone: Cardiology Day Ward (01482) 461517/ 461518, Ward 28 (01482) 461602, Ward 26 (01482) 461612