- Reference Number: HEY953-2024
- Departments: Endoscopy
- Last Updated: 1 April 2024
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
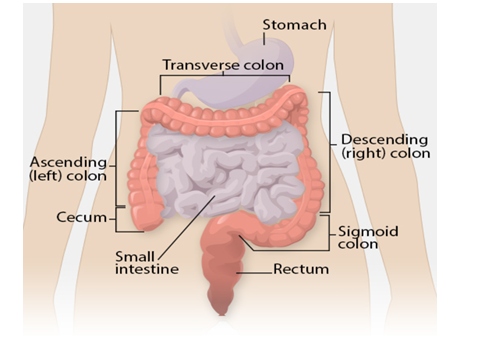
Where is the large bowel?
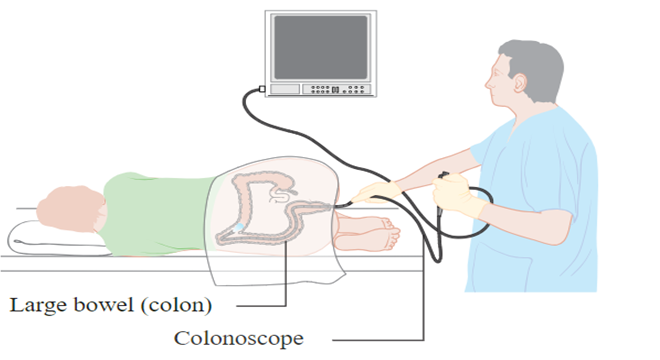
What is a Colonoscopy?
This is an examination of the large bowel using a long, flexible tube called a colonoscope. The tube allows the colon to be viewed directly and for pictures of the lining and samples of the tissues to be taken.
Why has this examination been arranged for me?
You will have seen your doctor regarding concerns about your bowels. Your doctor believes you may have a problem with your bowels and has referred you to the hospital to have some tests or to see a bowel specialist in a clinic.
Your doctor and/or your specialist feel that this examination (colonoscopy) is the best way to investigate your bowel (colon) problems. In this way the whole of the large bowel is seen at one visit.
The benefits of this examination include the ability to take biopsies to analyse parts of the large bowel lining which may be abnormal. It also enables the removal of polyps without the need (in the vast majority of cases) for an operation. Again this can usually be done at only one visit.
What happens if I refuse the Colonoscopy?
This is your choice and there might be alternative examinations we can use instead. Your plan of care and treatment may change, as it is possible that some important information will be unavailable.
Please discuss this with your consultant and endoscopist.
What are polyps and why is their removal so important?
Polyps are benign (not cancer) growths, which arise from the lining of the large bowel. They are very common and are often an unexpected finding during colonoscopy. Generally, they do not produce symptoms, but they tend to grow slowly over time and can occasionally turn into cancer. We cannot tell, just by looking, whether polyps contain cancer cells or not. They need to be removed and looked at under a microscope.
If the removal of polyps is unacceptable to you or you prefer to have them removed at a later date following further discussion with your doctor, please inform the endoscopist before you sign your consent and the examination begins.
Please read all the information sent to you by the Endoscopy Department.
Does a Colonoscopy have any risks I should know about?
Yes, there are. Risk means complications may occur. It is important to note that serious complications during colonoscopy are rare and for most people, colonoscopy is straightforward.
Feeling bloated
You may feel bloated (full of wind) and have stomach ache for a few hours after the test because air is blown into the bowel. You will find that this goes away when you pass wind.
We do keep a close eye on you in recovery and in the majority of patients these subside very quickly (15 to 20 minutes) but for some patients this can last a couple of days. Over this time bloatedness is common and comes and goes. As long as you are passing wind and going to the toilet, this will settle down.
Breathing and blood pressure
If you have sedative drugs, they can cause your breathing to slow down or lower your blood pressure. This is the reason we do not give high doses of the drugs for this test. We monitor your breathing and oxygen levels carefully throughout the procedure and this rarely becomes a problem. We can give a drug (antidote) to reverse the effects of the sedative straight away if needed. If you have a known allergy or reaction to sedatives and anaesthetics, please let the endoscopist and/or your nurse know.
Perforation (tear in the bowel wall)
There is a risk that the colonoscopy can tear (perforate) the bowel wall. The risk of this is less than 1 for every 1.000 tests done. A perforation can sometimes settle with antibiotics and resting your bowel, but an operation is usually required to repair the damage.
The risk of perforation is higher if polyps are removed. The level of risk depends on the size and location of the polyp. If removal of the polyp would be a higher risk procedure, the endoscopist may decide to simply take samples from it and ask you return to have the polyp removed at a later date. This will allow you the opportunity to discuss risk in more detail first.
Bleeding
It is common to have some bleeding from your bottom after colonoscopy. This should only be ‘spotting’ on the toilet paper or drops in the toilet bowl. It may take some days for this to subside.
Bleeding may happen when a biopsy or polypectomy is performed. This usually occurs during the procedure itself but may occur up to 14 days later. Usually the bleeding is minor, and stops on its own, rarely the bleeding can be more severe and may require admission to hospital and/or a blood transfusion. Very rarely a further colonoscopy or even surgery may become necessary to stop the bleeding.
Missed abnormalities
Rarely, if the bowel preparation has not worked very well and there is still stool in your bowel, polyps and even cancers can be difficult to see during the test.
Incomplete procedure
In certain situations, an endoscopist will encounter difficulty in advancing the colonoscope through the colon, leading to an incomplete procedure. This can happen in 1 in 10 cases. An incomplete examination may result in the colonoscopy being repeated or alternative tests arranged to examine the bowel.
Are there any alternatives to this procedure?
CT Colonography (Virtual Colonoscopy) This test is an alternative way of looking at your bowel. The main drawback of these is that they only provide pictures of the shape of your bowel and do not allow samples to be taken or polyps to be removed. You may need similar medicines to clear your bowels for these tests. Your Doctor or Nurse will have considered alternative tests for you before asking you to have a colonoscopy.
If you have questions about these alternatives, please mention them to your doctor.
How do I prepare for the colonoscopy?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination. Complete the health questionnaire sent/given to you as fully as possible.
To be able to see the lining of the large bowel you will need to have your large bowel empty and free of faeces. To do this you will need to change what you normally eat, and drink a powder to mix with water. Instructions for how to take these sachets and when to eat and drink should have come with your appointment time.
Please read the instructions carefully.
If you have diabetes (especially taking insulin) or you have serious heart, lung or kidney problems, or concerned that a health problem you have may be affected, then contact the Endoscopy Department at the hospital where you are having your examination (see contact numbers).
- CJD (commonly known as mad cow disease) – Please inform the department if you have been notified that you are at risk of CJD/vCJD (Creutzfeldt-Jakob disease/variant Creutzfeldt-Jakob disease) for public health reasons.
- PREGNANCY – It is important that you inform us if there is a possibility that you may be pregnant. Any information you share with us will be kept strictly confidential.
- MEDICAL DEVICES – If you have a pacemaker or implantable cardioverter defibrillator (ICD) please contact the Endoscopy Department at the hospital where you are having your examination (see contact numbers).
Due to the nature of the examination we ask you to change into a hospital gown. Although a gown and privacy shorts are provided, you may also wish to bring a dressing gown with you.
If your health has deteriorated whilst waiting for this examination, please inform your Endoscopy Department.
Where will I have my Colonoscopy?
The colonoscopy will be performed in the Endoscopy Department. It will be done at Hull Royal Infirmary or Castle Hill Hospital depending on where your consultant is based. Please make sure you go to the correct Endoscopy Department. Directions will be given with your appointment letter.
All the staff will endeavour to make your stay as easy and dignified as possible. Please do not be afraid or embarrassed to ask questions.
Who will perform my colonoscopy?
It may be your consultant, or another Colonoscopist, in these cases, your consultant will be sent a copy of the result.
This Trust is a teaching hospital and has commitments to train both doctors and nurses in all aspects of endoscopy and care. Occasionally doctors and/or nurses who are undertaking colonoscopy training may perform your procedure. An experienced endoscopist will supervise them. Your permission will be requested in advance for this. You may decline and the supervising endoscopist will perform the endoscopy.
Should I take my tablets during my bowel preparation and before coming for my Colonoscopy?
If you are taking tablets prescribed by your doctor or other specialist, you should continue to take these as normal. There are some medications that may need to be stopped or reduced for a period of time before your colonoscopy. Please see the instructions included with your appointment.
If you are taking any of the following medications, please contact your Endoscopy Department for further advice and instructions.
CLOPIDOGREL (PLAVIX), TICAGRELOR, PRASUGREL – These are blood thinning medications. Please inform the department if you are taking these tablets as these may need to be stopped prior to your procedure.
RIVAROXABAN, DABIGATRAN, APIXIBAN – These are blood thinning medications and usually have to be stopped for a period of time to reduce the risk of bleeding.
WARFARIN – These are blood-thinning tablets and usually have to be stopped for a period of time before colonoscopy due to the risk of bleeding.
IRON – If you take iron tablets then these are usually stopped for one week before the colonoscopy. Iron coats the inside of your large bowel making it very dark and difficult for the endoscopist to see anything. It is important to stop iron otherwise your colonoscopy will be cancelled and another appointment made.
MEDICATIONS FOR DIABETES – Adjustments to your regular medications for diabetes may need to be made, if you have not already received instructions, please contact the endoscopy unit.
Will the Colonoscopy be painful?
Discomfort can vary from person to person. You may feel some pressure, bloating or cramping as the camera moves through your colon. To make you as comfortable as possible during your procedure you will be offered a choice of medications.
Conscious sedation
Conscious sedation is where the sedative and a painkiller are given into a vein. This will make you more relaxed and reduces any discomfort experienced during the procedure. The sedative may also make you forget parts of the test. Each patient will react differently and will experience different levels of sleepiness. It is not a general anaesthetic and you will be awake during the procedure. To be able to do this a needle is inserted in a vein in your hand or arm. This is removed once the examination is finished and you have recovered.
If you have conscious sedation an adult friend, relative or carer must escort you home. You must also make sure that an adult stays with you for 24 hours after your procedure. Please make sure that you have access to a telephone when you return home. If you have not been able to make these arrangements, please speak to the nursing staff. We will not be able to give you sedation if you do not have someone to accompany you home.
Entonox®
Entonox® is commonly known as ‘gas and air’. This is a mixture of gases which is breathed in (inhaled). It is a quick acting painkiller that wears off quickly. We will show you how to use the mouthpiece before the colonoscopy starts and ask you to inhale the Entonox®. The effects are noticeable within 30 seconds. You can continue to inhale the Entonox® during the procedure. Unlike sedation, you can drive home 30 minutes after your procedure. Entonox® cannot be given to patients with some lung conditions or those who have had recent eye or brain surgery.
What happens to me in the Endoscopy Unit?
Our friendly staff will greet you on arrival. They will let your nurse know you have arrived. If there are any delays you will be notified as soon as possible and be kept informed.
We will ask questions about your general health and work through the health questionnaire that you kindly completed for us. Please feel free to ask questions.
We will check your blood pressure, pulse and oxygen levels, before your colonoscopy.
Your endoscopist and nurse will discuss the examination with you and will answer any questions you or a family member has. You will then be asked to read and sign the consent form.
If you need glasses to read, please keep them with you at all times do not leave them with a relative or tucked away in a bag or pocket.
You are then taken through into the examination room and asked to lie on your left side on the examination trolley.
Once in position, your nurse will attach a finger probe, which monitors your oxygen levels and pulse throughout and after the examination.
If conscious sedation drugs are administered, they may cause your breathing to become slow and shallow; therefore we will give you a little oxygen via nasal tubes.
How will I feel during and after the Colonoscopy?
This is just for information but may be very useful to your partner and family. The sedation we give may cause you to forget some or all of the examination. This varies from person to person. You may not remember much about it.
At first the endoscopist will examine your bottom with a finger. This allows lubricating jelly to be applied and to examine the first few centimetres of the large bowel, which is sometimes not seen by the camera.
When the camera is inserted into your bottom, air is gently passed into the bowel.
This opens up the bowel so the endoscopist can see where he/she is going. At first you may feel that you want to go to the toilet. You may feel a little anxious and embarrassed that you will pass a motion.
DO NOT WORRY
The first part of the large bowel begins to stretch. This sends messages to your brain telling you to go to the toilet. It is the air that causes this feeling.
Discomfort varies from person to person. It may be an ache and you may feel bloated, especially under the ribs. Instinct tells you to hold your breath until it passes. Try to relax and control your breathing, with good gentle, slow deep breaths. Your nurse looking after you will help.
Sometimes it can be quite painful. You must let your nurse and the endoscopist know. We can stop and remove some air, or change your position. The colonoscopy takes about 30 to 40 minutes.
What happens when the colonoscopy is finished?
You will be transferred to the recovery room. Here a nurse will continue to monitor your recovery this will involve checking your blood pressure, pulse and oxygen levels at regular intervals.
Gradually, as you recover, you will be advised to get rid of any ‘wind’ that may be trapped in your large bowel. We do appreciate that this can be embarrassing but it is important you do ‘let it go’.
You will eventually be able to sit up and you will be offered a drink. As you continue to recover you will be able to get dressed fully again and rest in a chair where you will be offered a drink and a biscuit.
Please take care. Initially you may feel dizzy and a little disorientated when getting off the examination trolley.
If you live alone or you do not have anyone who can be with you, please contact your Endoscopy Department so that other arrangements can be made.
Do I really need someone with me after colonoscopy?
If you have conscious sedation, yes, this is very important. The sedation given can have effects, which last some 24 hours after the colonoscopy. You can become forgetful and also sleepy again.
Your test may be cancelled if you do not arrange to have someone to collect you and stay with you for the next 24 hours.
If you have conscious sedation we strongly recommend that for the next 24 hours you:
- Do not drive
- Do not return to work or operate machinery
- Do not sign any important/or legal documents
- Are not left alone, you may be at risk of injuring yourself
- Are not left alone to care for children
Will I be told what was found and what happens next before I leave the Endoscopy Unit?
Yes. Your nurse and the endoscopist will explain the results to you. Due to the sedation you may forget what has been said. This is why it is important to have someone with you. The information will be written down and further supporting patient information leaflets will be given if required.
Further information
If you require further information about your test your GP, consultant, and the Endoscopy Department are a valuable source of information.
Useful contact numbers:
- The Endoscopy Department, Castle Hill Hospital – Telephone: 01482 622069 (direct line) – Monday to Friday, from 8:00 am to 5:00 pm
- The Endoscopy Department, Hull Royal Infirmary Telephone: 01482 674790 – Monday to Friday, from 8:00 am to 5:00 pm
- Ward 100 Hull Royal Infirmary – Out of hours: Telephone: 01482 674860
What do those words in the leaflet mean
Biopsy – A sample of tissue is taken for analysis.
Caecum – The first part of the large bowel; this is joined to the small bowel.
Consent – This is the agreement between you and the endoscopist. You are agreeing to have investigations or treatment and that you understand the purpose, benefits, alternatives and risks. You and the endoscopist during this process usually sign a consent form.
Colonoscopy – The examination of the inside of the large bowel using a long, flexible camera.
Endoscopy Department – The place where your procedure takes place
Colonoscopist – This can either be your consultant, an experienced and trained doctor or an experienced and specially trained practitioner.
Perforation – A rare, but possible risk in which a hole or tear is made through the large bowel.
Polyp – A common, benign (not cancer) growth arising from the lining of the large bowel. They take some years to develop. Some polyps, depending on their size and type, have the potential to turn cancerous.
Polypectomy – The removal of a polyp usually performed at the same time as the colonoscopy.
This leaflet has been written with the help, support, advice and collaboration of:
- Consultants in the Academic Surgical Department and the Department of Colorectal Surgery
- Consultants of the Department of Gastroenterology
- Staff of the Endoscopy Departments at Castle Hill Hospital and Hull Royal Infirmary.
- The patients and carers who have shared their experiences of colonoscopy with me and helped in auditing the information produced for readability, understanding and user-friendliness.
The patient pictures have been released as part of an open knowledge project and are reproduced with the permission of Cancer Research UK. Wikimedia Commons https://commons.wikimedia.org/wiki/Main_Page
Please see below the link to the Checklist that you will be asked to fill in and take to the clinic with you.
Colonscopy Information Checklist

