- Reference Number: HEY1106/2020
- Departments: Radiotherapy
- Last Updated: 22 April 2020
Introduction
This leaflet aims to help you and your family understand more about chemo-radiotherapy treatment for rectal cancer.
Before you agree to have treatment you should have a good understanding of the procedure and the possible side effects. This leaflet should support the discussion you have with your clinical oncologist (a doctor specialising in cancer treatment) and the rest of the team. Your team will include therapeutic radiographers (specialist staff who deliver radiotherapy) and nurses. Please ask if you have any questions or concerns which have not been answered or if you hear any words or phrases that you do not understand.
If you have any additional needs (physical, religious, cultural, emotional or medical), please inform a member of staff so that every effort can be made to meet your needs.
Once the treatment and its risks have been explained to you, you will be asked to sign the consent form. Signing the consent form still allows you to stop your treatment, though it is advisable to complete the course. If you are considering stopping treatment please discuss this with your oncologist.
What is rectal cancer?
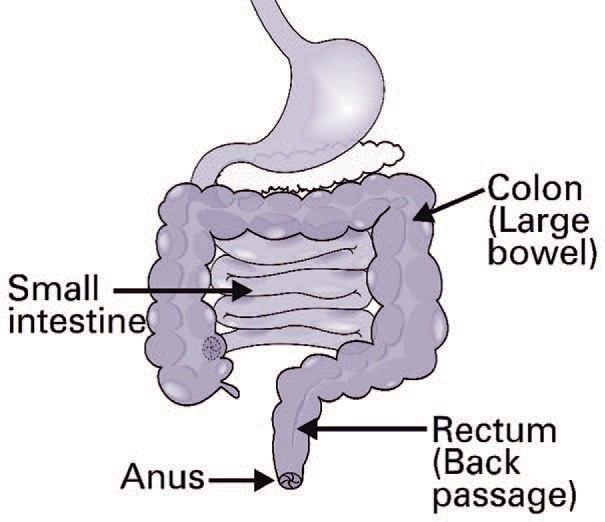
The bowel is part of the digestive system and is divided into two parts: the small and large bowel.
The large bowel is made up of the colon and rectum (back passage).
Waste food matter (faeces) is held in the rectum until it is ready to be passed from the body through the anus as a bowel motion (poo/stool).
A cancerous (malignant) lump that starts in the back passage is called a rectal cancer. A diagnosis is usually made after a physical examination and colonoscopy (a procedure which involves a flexible scope being passed through the anus into the bowel to view the inside of your back passage). A small amount of tissue (biopsy) is taken from the lump and sent to the laboratory for testing. This is usually followed by a number of tests, including scans and blood tests, to see if the cancer has spread to other parts of the body.
How is it treated?
Many cancers of the rectum are treated with surgery. In some cases, such as yours, we recommend a course of radiotherapy and chemotherapy either before, or occasionally after the operation. This decision is made after considering a number of factors including what the tumour looks like on your scan e.g. its size and location in the rectum.
What treatment will I receive and what is it called?
The name of your procedure is chemo-radiotherapy for rectal cancer. Chemo-radiotherapy is the use of both anti-cancer drugs (chemotherapy) and radiotherapy (high energy x-rays) in order to treat cancer.
Treatment will be daily apart from weekends, over five weeks, with chemotherapy usually given as tablets and taken on the same days as radiotherapy.
What are the benefits of this treatment?
The aim of treatment is to shrink the cancer before surgery. By shrinking the cancer it increases the chances of it all being removed during surgery. The treatment also aims to try and reduce the chances of cancer coming back again in the pelvis.
This leaflet will describe the radiotherapy treatment in detail. The chemotherapy aspect of your treatment will be explained in a separate leaflet.
What is radiotherapy?
Radiotherapy is the use of high energy x-rays, to treat cancer. The organs and tissues of your body are made up of tiny building blocks called cells. Radiotherapy causes damage to the cancer cells in the treatment area. Although normal cells are also affected, they can repair themselves and are able to recover over time. There is however a risk of permanent damage to normal tissues, this will be explained further in the side effects section of this leaflet.
Radiotherapy itself is painless and does not make you radioactive. It is perfectly safe for you to be with other people, including children throughout the duration of your treatment. However, only you can be in the treatment room when the radiotherapy machine is on.
Treatment is delivered by a machine called a linear accelerator, also known as the treatment unit or LINAC, shown in this photograph.

Planning your treatment
After seeing your doctor in clinic you will receive an appointment to visit the radiotherapy department at Queens Centre, Castle Hill Hospital for radiotherapy planning.
Your first radiotherapy appointment may include:
- Having a ‘planning’ CT scan
- Signing the consent form
- Having blood tests
CT scan
As part of your treatment you will need to have a planning CT scan which is used to identify where the cancer is. This is so that your radiotherapy can be accurately delivered to this area. The planning scan usually takes 10-15 minutes. You will be asked to undress from the waist down. Before the scan you may be asked to drink water so that your bladder is comfortably full. This is to help reduce side effects to your small bowel.
Some patients will also be given an injection in their arm of a contrast fluid; this helps us plan your radiotherapy. The contrast is only needed for this scan, not each treatment.
The scan is taken with you lying flat. You will be required to stay very still in this position for each treatment, so it is important that you are as comfortable as possible. If you find this position uncomfortable then please let the radiographers know.
Once you are in position, the radiographers will ask your permission to draw some marks on your skin. The marks are used as a reference point and help place you in the correct position for treatment each day. At the end of the scan these marks will be replaced by permanent marks. The marks (tattoos) are no bigger than a freckle and will be used each day for your treatment. You can wash as normal without worrying about the marks coming off.
The process of planning your treatment can take about 2-4 weeks.
At this appointment a member of the radiotherapy team will meet you to discuss and explain the possible side effects. They will also provide advice on how to minimise them and answer any questions or concerns you may have.
What should I expect on the day of treatment?
When you arrive for radiotherapy you should go to the radiotherapy department and book in at the reception desk. You will be asked to take a seat in the waiting area.
You can expect to spend 10-15 minutes each day in the treatment room. The treatment machine is only switched on for a fraction of this time. For most of the time the radiographers are carefully placing you and the machine in the correct position for your treatment. You will be on your back in the same position you were in for your CT planning appointment. The machine does not touch you. It is important for you to stay as still as possible but breathe normally. Once you are set up in the correct position the staff will let you know that they are leaving the room for a few minutes to start treatment.
The machine is controlled by staff outside in the ‘control area’ and the machine will rotate around you in different directions. The radiographers are watching you at all times on their television monitors. If you feel you want to stop the treatment at any time, just wave to attract their attention, they will be able to see you on their monitor. If you do need attention the machine will be stopped and the radiographers will come back into the room. The television images on the monitor are not being recorded or saved.
You will not feel or see anything during treatment however you may hear a buzzing sound when the treatment is being delivered.
You will have several sets of images taken during your treatment to ensure that the radiotherapy is being delivered accurately to the right area. These images are necessary, but will result in a small dose of additional radiation which has been agreed by your doctor. Any risk from this dose is far outweighed by the benefits to you during your radiotherapy.
Chemotherapy
You will be required to have chemotherapy on the days you have radiotherapy. This will be administered as a course of tablets (Capecitabine) taken twice a day. Or it is given through a drip (5 Fluorouracil). An appointment will be made for you to have a pre-assessment talk with a member of staff to discuss how to take the tablets and also to collect them from the pharmacy. It will be another opportunity for you to ask any questions about the treatment.
You will be required to sign a separate consent form for chemotherapy where its side effects will be described in more detail.
What are the side effects and complications of chemo-radiotherapy?
Side effects can be divided into short term effects that happen during or soon (weeks) after treatment and long term effects which can occur months or years later. Both chemotherapy and radiotherapy can be responsible. Some are common; others are potentially serious but rare.
Below is a list of side effects along with how likely it is for that particular side effect to occur. Here are some definitions to help you:
- Common – More than 10 in every 100 (>10%) people will develop this side effect
- Occasional – Between 1 and 10 in every 100 (1-10%) people will develop this side effect
- Rare – Less than 1 in 100 (<1%) people will develop this side effect
However, please be aware that each patient can react differently to treatment and you may experience side effects at different times and to varying degrees, compared to other patients having the same treatment.
Short term side effects
Bowel problems:
Radiotherapy includes treating some of your normal bowel as well as the cancer. It can cause inflammation and these specific side effects:
- Common
- Diarrhoea (i.e. more liquid stools, that are passed more often). If you have a stoma you may need to change or empty your bag more often.
- Abdominal bloating and discomfort
- Bleeding or mucus loss from the rectum
- Feeling of fullness in the rectum or pain (particularly if your tumour is low down)
- Occasional
- Needing to get to the toilet quickly (urgency)
Bladder problems:
Your bladder will also be included in the treatment area (as it is very close to the rectum), causing these side effects:
- Common
- Pain/stinging on passing urine
- Passing urine more often
- Occasional
- Needing to get to the toilet quickly (urgency)
Tiredness (fatigue)
- Common
- Nearly all patients undergoing chemo-radiotherapy will feel more tired than usual. This can be most noticeable towards the end of treatment and often continues for a short number of weeks after its Fatigue is usually a combination of the side effects and attending hospital every day. Be prepared to rest when necessary during treatment.
- Rare
- Whilst some fatigue is common it is rare for it to prevent being able to do day-to-day tasks or drive.
Skin and hair changes
- Common
- The skin in the treated area (front and back) may become red and sore, but this varies from person to person. Before starting treatment you will have a chance to meet one of our radiotherapy team to discuss the latest skin care advice.
- Having radiotherapy prior to surgery can sometimes mean that wounds take longer to heal (particularly if your tumour is low down in the rectum).
- You may lose pubic hair in the treated area, but it will grow back once treatment is complete.
Life threatening complications:
Rarely a patient can die whilst undergoing chemo-radiotherapy. This is usually due to rare complications of the chemotherapy (Capecitabine or 5 Fluorouracil) as outlined below:
- Rare
- Infection: Chemotherapy temporarily reduces the production of various parts of your blood. Most importantly, it can reduce your ability to fight infection. It is important to understand that any feverish illness during treatment can be much more dangerous than normal. You are advised to have a thermometer at home and contact the hospital for advice if you become unwell (please check your temperature beforehand). You will be given the number to ring if this happens. Symptoms to watch out for include:
- Shivering when others are warm
- Uncontrollable shaking
- Suddenly becoming unwell over just a few hours
- Sensitivity to chemotherapy: A very small proportion of the population are particularly sensitive to the chemotherapy used in this treatment. If you experience significant side effects (such as diarrhoea and nausea) early on in the treatment (especially within the first week to 10 days) then this is unusual and may be a warning sign that you are one of these individuals. You should stop taking the tablets and ask for help straight away if this happens.
- Chest pain: You must do the same if you develop unusual, persistent chest pain (especially if it is associated with shortness of breath), as the treatment can occasionally affect the heart. If this happens you should seek urgent medical advice.
- Skin reaction: Very rarely (in fewer than one in ten thousand patients treated) Capecitabine has been shown to cause a severe and sometimes fatal allergic condition with blistering or breakdown of the skin, eye problems and effects on the internal Sometimes we stop chemotherapy part way through treatment if a patient develops significant side effects.
- Infection: Chemotherapy temporarily reduces the production of various parts of your blood. Most importantly, it can reduce your ability to fight infection. It is important to understand that any feverish illness during treatment can be much more dangerous than normal. You are advised to have a thermometer at home and contact the hospital for advice if you become unwell (please check your temperature beforehand). You will be given the number to ring if this happens. Symptoms to watch out for include:
Long term side effects
The long term effects that you experience can depend on the type of surgery you have. In some cases, it is surgery that is the most likely cause of the problems outlined below. Your surgeon will advise you on the most appropriate surgery for you. Some people will have a stoma which may be permanent or temporary and some may undergo complete removal of the back passage at surgery. In others, the bowel is joined up again and they pass a motion in the normal way.
Bowel problems
- Common
- Permanent change in bowel habit – having your bowels open more often.
- Urgency to get to the toilet and not being able to control it (faecal incontinence) which may cause soiling of clothing or leakage.
- Recurring (chronic) abdominal pain and pain in the
- Occasional
- Risk of bowel damage requiring surgery and a stoma (if you do not already have one).
- A fistula (false passage between the bladder and/or vagina and bowel) or narrowing of the bowel (stricture).
Bladder problems
- Common
- Needing to pass urine more often.
- Occasional
- Not being able to control your bladder as well – causing dribbling and leakage.
Sexual dysfunction (Women)
- Common
- For female patients who have not gone through the menopause, this treatment is likely to induce the menopause and infertility (so you will no longer be able to have children). We can refer you to a specialist to discuss the storage (freezing) of eggs or embryos, which could potentially be used in future.
- Women may also notice their periods becoming irregular during or after treatment.
However, you should continue to use contraception during your treatment and for one year after your treatment has finished.
Since both chemotherapy and radiotherapy may harm an unborn child it is very important to avoid pregnancy during treatment.
- After treatment, some women experience vaginal dryness and pain during sex. You will receive a separate leaflet regarding feminine care during and after chemo-radiotherapy, including advice on the use of dilators to help this.
Sexual dysfunction (Men)
- Common
- If infertility is not caused by treatment it can affect the quantity and quality of sperm production. This can lead to increased rates of abnormality in children that are conceived during or after treatment. Men are advised to use contraception for one year after treatment.
- If you would like to have more children in the future, you should discuss this with your doctor before starting radiotherapy so we can arrange storage (freezing) of some sperm, this can then be used at a later time if needed.
- There is an increased risk of impotency (being unable to attain and maintain an erection) if you have received radiotherapy and If this is a problem, then you should discuss it with your GP or hospital team and you can be referred to a specialist clinic.
Skin changes
- Common
- Long term, the skin can look different in the treated area and feel You may notice pigment changes and the development of small blood vessels on the skin surface.
Second malignancy
- Occasional
- In the long term there may be a slightly increased risk of developing a new cancer caused by the treatment. Accurate information on this is not available and the benefits of the treatment far outweigh any potential risk in the future. If you are at all concerned then please speak to your medical team.
Bone health
- Occasional
- There is an increased risk of fractures of the pelvic and sacral bones after radiotherapy.
These are usually “hairline” and treated with painkillers.
Leg swelling
- Rare
- Pelvic radiotherapy and surgery may interfere with the drainage of fluid from the
legs, causing a degree of “puffiness” or swelling. However, this is a rare complication and there are other, more common, causes which would need to be considered if it occurs after treatment.
Is there anything else I need to be aware of?
During the course of your treatment it may be necessary to:
- Admit you to hospital, for instance if you develop infection.
- Undertake a blood or platelet transfusion (though this is very rare).
It is also worth being aware that the radiotherapy centre is a training centre for radiographers, so students may be present on the unit. However, they are supervised at all times. If you do not wish students to be present during your treatment then please speak to a member of staff. This will not affect your treatment or care.
Are there any alternative options to this type of treatment?
If your cancer is not currently operable then going straight to surgery without chemo-radiotherapy would not be recommended, as there is a chance some cancer would be left behind.
Chemo-radiotherapy aims to shrink the cancer, giving us the best possible chance of fully removing it through surgery.
If the cancer is operable at present, then it would be possible to proceed directly to surgery, but this could lead to an increased chance of the cancer coming back in the pelvis, than if you had chemo-radiotherapy.
What will happen if I decide not to have any treatment?
If you choose not to have any treatment, then it is likely that the cancer will continue to progress and in time cause you symptoms such as pain, bleeding and sometimes a blockage of the bowel. It is also possible that it can spread to other organs and probably shorten your life, although chemo-radiotherapy may not prevent this.
Will there be any follow up appointments?
At the end of your treatment the radiographers will give you advice and contact numbers. We will see you in the Outpatient Department 4-6 weeks after completion of radiotherapy by which time the short term side effects should be settling down.
Who should I contact if I have any other concerns?
For further advice please contact our Radiotherapy Information and Support Team:
• (01482) 461206
For out of hours emergencies (after 5.00pm and at weekends and Bank Holidays) call:
• (01482) 875875 ask for bleep 500
You can also call your specialist nurse or consultant’s secretary if it is not urgent.
Where can I find further information?
Radiotherapy Information & Support Team (01482) 461206
Macmillan Cancer Support 0808 808 0000 www.macmillan.org.uk
Bowel Cancer UK 0207 940 1760
NHS Smokefree National Helpline 0300 123 1044
Signing the consent form
Before we are able to undertake any medical treatment, test or examination we must first seek your consent. For some procedures we do this by asking you to sign a written consent form. It is important you fully understand what the procedure involves before you give your consent. The information in this leaflet aims to provide information about the procedure to help you make this decision. If you need more information or are unsure about any aspect of the procedure or treatment proposed please do not hesitate to ask for more information. Some questions you should consider include:
- What are my options?
- What are the pros and cons of each option?
- Do I need more information or support to help make this decision?
Please do remember that you are entitled to change your mind at any point, even after the consent form has been signed. If you do change your mind we recommend you discuss this with your oncologist.
This leaflet was produced by the Operational Delivery Network of Hull, Leeds and Sheffield Radiotherapy Centres.