- Reference Number: HEY1144/2020
- Departments: Ophthalmology Department, Orthoptic
- Last Updated: 19 December 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a tear duct?
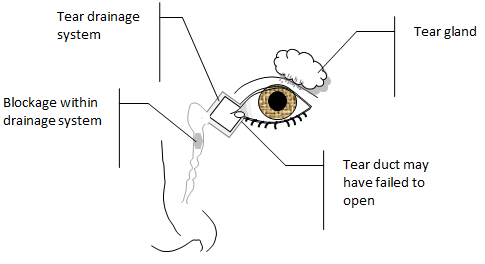
The eyes protect themselves by constantly producing tears to moisturise and wash away debris that falls onto the front surface of the eyes. The tear duct (nasolacrimal duct) is a tube connecting the inner corner of the eyelid to the inside of the nose. Its purpose is to drain tears away. Babies only start producing tears one or two weeks after birth. Sometimes at birth the tear ducts of one or both eyes do not fully open. This typically occurs in 1 out of 5 babies.
Why does it get blocked and what are the symptoms?
It is not entirely understood why in some babies the tear ducts do not fully open. Due to the tear ducts not fully opening the tears produced are unable to drain away. Tears can often pool in the corners of the eye or spill over on to the cheeks, it may be on one side or both, and it may be noticeable even when the child is not crying. Symptoms can sometimes become worse in colder weather, or if your child has a cold. Other signs may be your child waking up after sleeping with particularly sticky or crusted eyes. Children with blocked tear ducts can be prone to repeat eye infections.
Should I be worried if my baby has this?
No, blocked tear ducts do not directly have any implications on the development of your baby’s vision or eyes. In nine out of ten cases blocked tear ducts resolve on their own within the first year of life.
How can I help?
The majority of children with a blocked tear duct resolve on their own without the need for any form of intervention. If the tear ducts are not open at birth they may gradually open in the first few weeks or months of life on their own, without treatment. During this time there are things that can be done to keep your child comfortable. Due to the constant wetness around the eyes sometimes the skin can become sore; keeping the area dry and moisturising the skin can help. It is also important to be aware the eyes may develop conjunctivitis, (red, inflamed eye). If this happens antibiotic drops may be required.
If when the child wakes from sleeping you notice a slightly sticky or crusty appearance around the eyes, it will help to gently wipe this away with cooled boiled water using cotton wool.
If the problem persists you may be advised by a health professional to carry out massage of the area in order to encourage the tear ducts to open. You will be shown the most effective way to do this.
You must ensure you first wash and then dry your hands thoroughly. Then using your small finger, apply a small amount of pressure between the inner corner of the eyelids and outside bridge of the nose and slide your finger down towards the mouth. Carry out no more than ten strokes, and do this twice a day. This may help speed up clearing any blockage and opening up the tear ducts.
If this resolves the problem, then no further treatment is needed.
When should an operation be considered for blocked tear ducts?
In most cases the problem will have spontaneously resolved by 1 year of age. However, if the problem persists after this age or your baby has repeated eye infections, then an operation may be considered. The aim of the operation would be to open up the tear ducts to prevent the buildup of discharge and to help avoid infection. There is no necessity to have the operation, as there is still a chance the problem may resolve on its own by the age of 5 years.
Can there be any complications or risks?
There are risks with any surgical procedure due to the need for general anaesthetic. This procedure generally has a very low complication rate. It is a short day case operation in which a tiny probe will be used to open up the tear ducts.
What is important for me to know following the surgery?
Following this operation, nose bleeds can occur in the first few days. You will be advised to avoid encouraging your child to blow their nose for at least the first week after surgery. You may notice some slight bruising around the eyes and on the eyelids, but this typically settles within the first two weeks.
You will need to try and prevent your baby from rubbing their eyes following the procedure to minimise the risk of infection. You will also be asked to avoid getting any liquids such as soap or shampoo in your baby’s eyes. If the eyes become sticky you may need to clean the eyes with cooled boiled water and cotton wool.
Some babies may require a repeat operation if symptoms do not fully resolve after the first operation.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Orthoptic Department on telephone (01482) 816605.

