- Reference Number: HEY153-2024
- Departments: Pathology
- Last Updated: 1 January 2024
Please accept our sympathy for your loss
Introduction
This leaflet explains why you may have been asked to give your consent to a post-mortem examination at such a distressing time and explains the procedure.
We appreciate that you may not want to be given a large amount of information at the present time but if you do want more information, this leaflet is accompanied by a more in-depth guide. Staff are available to answer any questions you may have and to guide you through the consent form. Please feel free to ask any questions you may have at any time during the consent process.
What is a post-mortem?
A post-mortem, also known as an autopsy, is an important medical examination that seeks to find out more about a person’s illnesses and the cause of their death.
There are two types of post-mortem:
1. Post-mortem examination required by Her Majesty’s Coroner
This is an investigation required by law and does not require the agreement of relatives.
2. Consented post-mortem examination
This is an examination which can be either requested by you or by the consultant who was responsible for your relative’s care. Its purpose is to find out more information about your relative’s illness when the cause of death is already known. This can only be done with your full permission and you will have choices about the extent of the examination.
A consented post-mortem cannot take place without the agreement of the next of kin
If you agree to a consented post-mortem examination the doctors will issue the medical certificate of death before the post-mortem so that you can proceed with the arrangements for the funeral.
Why are post-mortems carried out?
Post-mortems are usually associated with establishing a cause of death, particularly in Coroner’s cases. When your consent is being sought for a post-mortem, there is usually no uncertainty regarding the cause of death though the underlying disease process may be poorly understood.
Post-mortems have far wider reasons for medical education and research generally. Examining tissue is one of the most important ways in which doctors learn about illness and how to treat it. Tissue from post-mortems can be used to train medical students and new doctors, to help experienced doctors continue to learn about new conditions or treatments, or to teach specialist knowledge.
New medical conditions are recognised all the time and the way in which medical conditions are classified and characterised changes as new technologies are developed. If tissue samples have been retained, it is sometimes possible to use this new knowledge to improve or change a diagnosis.
With your permission, an organ (or part of an organ) might also be retained for use in medical research or education. If the organ shows a particularly clear example of a specific illness, it may play an important role in the education of medical students, doctors and nurses.
Tissues and organs can only be retained at post-mortem with the express consent of the next-of-kin.
Donating organs for transplant is handled separately from the post-mortem procedure. Please ask if you would like any further information.
Tissues, blocks and slides
When you are asked for your consent the person obtaining consent will explain the procedure to you. This will include the necessity to retain tissue samples or whole organs, any requirements for genetic tests, photographs or X-rays and the reason of any limitations that you impose. You will be asked to complete a consent form, which gives detailed choices regarding the examination.
What happens to the tissue samples in the laboratory?
The small tissue samples will be placed into plastic cassettes.
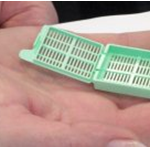
They are then processed into paraffin wax blocks in the laboratory. The blocks are normally about 20mm (millimetres) (less than one inch) square and about 5mm (millimetres) (under one quarter of an inch) thick.

The tissue is chemically treated to remove water, which is replaced with wax. The tissue ‘blocks’ become hard so that thin sections can be cut with a sharp knife. These sections are very thin – ten times thinner than a hair.

They are placed on glass slides and stained with special dyes to allow examination under a microscope. More than one slide may be cut from a block. This is exactly the same as occurs to samples taken during an operation.
During the process of making the blocks, it is usual that very small amounts of tissue will be surplus to requirements. These would normally be disposed of according to hospital policy, unless you have an objection to this.
Why is it useful for tissue blocks and slides to be kept?
Medical opinion recommends that the retained tissue blocks and slides are retained at the hospital where the post mortem examination was performed as part of the medical record. This is normally 30 years. This will allow them to be looked at again in the future should any questions about the cause of death be raised. Tissue blocks and slides can also be checked if any other member of your family has a similar medical problem.
Whatever your wishes for the tissue blocks and slides you will need to sign a consent form. This consent form also gives you the options to agree to retained tissues being used for training doctors, other teaching, ethically approved medical research, audit, public health surveillance and to assist in the diagnosis of other patients. Many people agree to this understanding that this may help other people with illness in the future. When tissue samples are used in this way, any information that can link them to your relative is removed.
When do post-mortems take place?
The post-mortem will be carried out as soon as possible, usually within two to three working days. It may be possible to arrange it within 24 hours if necessary.
Who conducts a post-mortems?
Post-mortem examinations are conducted by pathologists, who are specially trained doctors, with help from trained technical staff. They take place in the mortuary.
What is involved in a post-mortem?
A full post-mortem examination involves examination of each of the main body systems including the brain and all the contents of the chest and abdomen. It will normally include the removal and retention of small tissue samples for examination under a microscope.
Sometimes whole organs may be retained (with your consent) for closer examination. In some cases, organs and tissues may need to be temporarily retained for the preparation of blocks and slides – you will be advised if this is the case. You may have been asked to give written agreement for a specified organ or organs to be retained for diagnostic purposes by the pathologist.
If you agree, a hospital post-mortem can be limited to one body cavity (for example, the chest) or organ system (for example, the lungs), but this may not provide all possible information about the disease or cause of death.
What happens afterwards?
If you wish, you will be able to see your child, partner or relative’s body again after the post-mortem, before proceeding with your funeral arrangements. Usually the results of the examination will be available within about 12 weeks. A copy of the report will usually be sent to your relative’s GP or hospital consultant with whom you may wish to make an appointment to discuss the results.
If any organs or tissue had to be retained after the post-mortem for further examination, these can be returned to you or the funeral director once they are no longer needed, or disposed of by the hospital, whichever you prefer. Or you may choose to donate these for use in medical education or research.
If you choose to donate the organs or tissue for research, it is possible that the organisation receives the material may have to contact you again to get specific consent for the organisation to store it. It is also possible that tissues and organs donated for research may not be used as the material may not be suitable for the scientific projects that are occurring at any one time. You may have decided that any tissue or organs retained during the post-mortem examination are to be returned to the deceased. Please be aware that this will delay your funeral arrangements.
What if I change my mind?
We fully understand that this is a difficult time for you and that information given to you during the consent process may be unclear. This information leaflet should help to explain any concerns you may have but if you have any further questions or are uncertain about anything you have been told please do not hesitate in contacting the Mortuary on tel: 01482 608924
Once you have signed the consent form you will be advised when the post-mortem is to take place. You still have the right to withdraw your consent up to 10.00am on the day of the post-mortem.
If you do change your mind and wish to withdraw consent please contact the Mortuary on tel: 01482 608924 or tel: 01482 608928 and ask to speak to the Mortuary Manager or Mortuary Deputy Manager.
Explanation of terms
The most common words and terms used to describe what happens in a post-mortem examination are explained here. If you are unsure or require further information please do not hesitate in contacting the mortuary on the number(s) above.
Audit
Audit checks the standards of care and service. Some separate testing of tissue is needed to make sure that the standards of testing are of a high quality. Some tissue samples are needed for quality control of diagnostic tests, or to check on standards in a hospital pathology service.
Coroner
The Coroner is an independent judicial official responsible for investigating deaths. He or she is either an experienced lawyer, or an experienced doctor who has also had legal training.
The Coroner and Coroner’s Officers can be contacted at: Essex House, Manor Street, Hull, HU1 1YU. Tel: 01482 613009
Diagnosis, diagnostic use of tissue and diagnostic tests
Tissue samples are examined to find out as clearly as possible any specific illness the person had before they died. Looking at tissue with a microscope can identify diseases that could not be seen any other way, including those caused by genetic disorders. New medical conditions are being recognised all the time. If tissue samples have been retained, it is sometimes possible at a later date to diagnose these new conditions in cases in which they were previously undiagnosed, or given a different diagnosis.
Education (Medical Education, Teaching and Training)
Examining tissue is one of the most important ways in which doctors learn about illness and how to treat it. Sharing information between doctors is important in maintaining high standards of care. Students and doctors in training need to observe and learn about post mortem examinations and to discuss the procedure and findings with an experienced doctor.
Fixing
This is the preparation of tissue or whole organs for further testing by preserving with chemicals.
Full post-mortem Examination
A full post-mortem examination involves examination of each of the main body systems including the brain and all of the chest and abdomen. It will normally include the removal and retention of small tissue samples for examination with a microscope. Sometimes whole organs may be retained for closer examination but only with your consent.
Limited post-mortem Examination
If you wish, a hospital consented post-mortem can be limited to one body cavity (for example, the chest) or organ system (for example, the lungs). This may not provide all possible information about the disease or cause of death.
Organ
A part of the body composed of more than one tissue that forms a structural unit responsible for a particular function (or functions). The body contains many organs, such as the brain, heart, lungs, kidneys and liver.
Post-mortem
The Latin phrase ‘post-mortem’ means ‘after death’. A post-mortem examination is a medical examination after a person’s death, also known an autopsy. Post mortem examinations are done by pathologists, who are specially trained doctors, with help from fully trained technical staff.
Retaining or retention of tissue and/or organs
Sometimes one or more whole organs, part of an organ or tissue samples are kept after the post-mortem examination in order to reach a diagnosis. Reasons for this are:
- The organ or part of it may need to be examined with a microscope.
- The organ may show signs of a complex abnormality that requires a more detailed examination, perhaps by another specialist.
- The tissue or organ may need to undergo preparation before it can be examined. Preparation may take several days and sometimes many weeks.
With your permission, an organ (or part of an organ) might also be retained for use in medical research or education.
If the organ shows a particularly clear example of a specific illness, it may provide an important role in the education of medical students, doctors and nurses.
Tissue
A collection of human cells specialised to perform a particular function. Organs contain tissues. For example, the heart contains muscle tissue composed of cells that contract to pump the blood around the body. In addition, it also includes blood vessels, fat and nerves.
Tissue Samples, blocks and slides
To understand an illness or cause of death properly, the doctor needs to look at part of the affected organ under the microscope. To do this, small samples of tissue are taken from the organ (usually about 1 cm across and about 5 mm thick). These samples are made into hard blocks using wax. From these, very thin sections, 10 times thinner than a human hair, can be cut off. They are placed on glass slides so that they can be examined under a microscope. More than one section can be cut from one block.
Should you require further advice on the issues contained within this leaflet, please do not hesitate to contact the Mortuary on tel: 01482 608924 or tel: 01482 608928 and ask to speak to the Mortuary Manager or the Deputy Mortuary Manager.

