- Reference Number: HEY1588/2025
- Departments: Orthopaedics, Therapies
- Last Updated: 31 October 2025
Introduction
This leaflet has been produced to give you general information about how to care for your hip following surgery. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is a broken hip?
Your hip is classed as a ball and socket joint and is located where your thigh bone (femur) meets your pelvis (acetabulum). A broken hip is referred to as a neck of femur fracture.
Each year, over 70,000 people in England, Wales and Northern Ireland sustain a hip fracture with this figure continuing to rise due to an ageing population.
Why do I need hip surgery?
Due to the nature of your hip fracture, the medical team may advise that you need an operation to fix the fracture. This will help to stabilise the fracture and help with the recovery process. Additional benefits can include:
- Relieve pain from the injured hip joint
- Increase quality of life
- Improve the function of the hip joint
- Increase mobility
What are the types of surgery to fixate a hip fracture?
Total hip replacement
Involves removing the head of the femur (round ball at the top of the thigh bone) and the acetabulum (hip socket), replacing with prosthetic components. See separate leaflet titled ‘Your Guide to: Total Hip Replacements’
Copyright by AO Foundation, Switzerland
Source: AO Total Hip Arthroplasty, https://surgeryreference.aofoundation.org/total-hip-arthroplasty
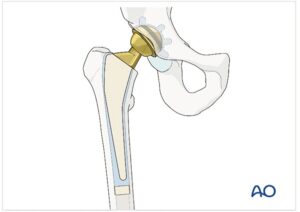
Hemiarthroplasty
Involves removing the head of the femur and replacing it with prosthetic components. The hip socket is not removed during a hemiarthroplasty. A hemiarthroplasty is often referred to as half a hip replacement.

Copyright by AO Foundation, Switzerland
Source: AO Hemiarthroplasty, https://surgeryreference.aofoundation.org/hemiarthroplasty
Dynamic hip screw
Involves inserting an artificial plate and screws into the femur (thigh bone) and a large screw into the head and neck of the femur.
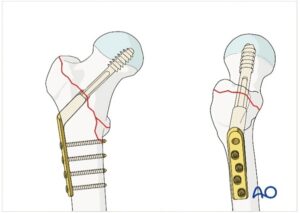
Copyright by AO Foundation, Switzerland
Source: AO Sliding hip screw, https://surgeryreference.aofoundation.org/sliding-hip-screw
Intramedullary nailing
Involves inserting a long nail into the intramedullary cavity of the femur.
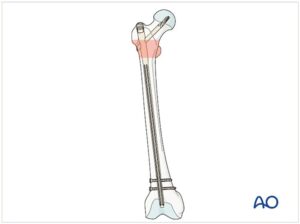
Copyright by AO Foundation, Switzerland
Source: AO Nailing (long nail), https://surgeryreference.aofoundation.org/nailing-long-nail
Cannulated hip screw
Involves inserting screws through the neck of the femur into the head of the femur.
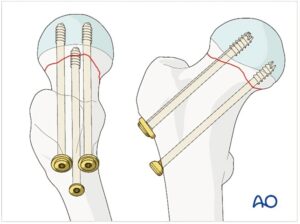
Copyright by AO Foundation, Switzerland
Source: AO Cannulated screws, https://surgeryreference.aofoundation.org/cannulated-screws
Open reduction internal fixation (ORIF)
Involves inserting internal fixation devices e.g. plate and screws to fixate the fracture.

Copyright by AO Foundation, Switzerland
Source: AO ORIF, https://surgeryreference.aofoundation.org/orif
What are the risks of hip surgery?
As with any surgical procedure, there are risks which you will have been informed about by the medical team prior to your operation. Examples of risks include:
- Blood clots – to reduce the risk of blood clots, you will be assessed for and given blood-thinning medication where appropriate. You may also be given thromboembolic deterrent (TED) stockings for your legs.
- Stroke/heart attack/heart failure – the stress on the cardiovascular system from surgical interventions can increase the risk of these events occurring.
- Swelling – swelling after surgery should subside over time but rates can vary between patients. To help reduce the swelling, elevate the limb.
- Neurovascular damage – the healthcare team will monitor this by checking your sensation, movement and blood flow to the limb following surgery.
- Infection – please report any wound leakage, redness, heat, increasing pain and/or discharging pus to the healthcare team.
- Leg length discrepancy – occasionally following surgery, there can be a difference in your leg length. A referral to orthotics would be made by your medical or therapy team for this to be reviewed and treated.
- Dislocation – exercises can help strengthen the soft tissue structures around the joint to help reduce this risk.
- Loosening and failure of metalwork – over time, the artificial components can loosen and wear out, potentially leading to further surgery.
How do I prepare for hip surgery?
Please read this information leaflet. If you wish, please share the information it contains with your family so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following the surgery.
You will be unable to eat and drink prior to the surgery to reduce the risk of complications from the anaesthetic. The healthcare team will be able to advise you further regarding this.
The medical team may place you on bed rest until the surgery has been performed. Regular movement of your non-injured limbs is important to help reduce the risk of muscle shortening, limb weakness and blood clots. The therapy team can provide you with bed exercises to complete prior to the operation and may also provide some deep breathing exercises to help reduce the risk of chest infections.
What will happen before hip surgery?
Following your injury, you are likely to be admitted to the hospital via Accident and Emergency (A&E) where you will be assessed and admitted onto a ward.
Upon being transferred onto the ward, the healthcare team will admit you and take note of your: reason of admission, clinical diagnosis, review imaging such as x-rays, past medical history, prescribed medication, social history and any other details deemed relevant.
The medical team will review your case and decide on the best surgical option for you. They will have a conversation with you regarding why they have chosen this and explain the risks and benefits. You will then be asked to sign a consent form.
Before you go to surgery, you will undergo a standard surgical checklist assessment. The healthcare team will run a variety of tests such as an electrocardiogram (ECG) and an infection screen. They will perform blood tests including full blood count, urea and electrolytes, C-reactive protein (CRP), group and save, bone profile, liver function test and vitamin D. They will perform clinical observations and ensure your medication and fluid balance chart is up to date. They will also ensure VTE prophylaxis has been completed. An anaesthetist will assess you for the appropriate type of anaesthetic.
Exercises
Whilst you are awaiting surgery, the therapy team will encourage you to complete some bed exercises. The exercises will help to improve your circulation, maintain your muscle strength and range of movement.
Complete the following exercises on the unaffected side throughout the day. On the affected side, complete the ankle exercises as pain allows and focus on upper limb range of movement and strength.
- Ankle Pumps – slowly move your foot up and down. Complete 3 sets of 10.

- Knee flexion/extension – slide your foot toward your buttocks, bending your knee and keeping your heel on the bed then straighten your knee back out and press it down into the bed and hold for approx. 3 to 5 seconds. Complete 3 sets of 5.

- Straight leg raise – tighten your thigh muscles with your knee fully straightened on the bed and then lift your leg several inches. Hold this for 5 to 10 seconds. Complete 3 sets of 5.

More specific exercises can be provided following your operation to ensure the exercises are individualised to your needs.
Therapy Questionnaire
The therapy team will ask you to complete a questionnaire with them about your social history. This is used to determine your set up at home and any support/equipment you might already have in place. For example:
- Who do you live with?
- Is this in a house/bungalow/flat?
- What is the access like? Any steps and grab rails?
- How were you mobilising pre-injury? Were you using any walking aids?
- How were you managing? Did you need family support or a package of care?
- Do you have any equipment in situ? Anything to help you in/out of bed or on/off the toilet?
What to expect
- Your leg will be ‘marked’ for the operation by drawing an arrow pointing to your hip.
- You are not allowed to eat or drink from midnight prior.
- You will usually have a general anaesthetic when undergoing hip surgery, but this will be decided by the anaesthetist.
- You are likely to be off the ward for approx. 2 to 6 hours although the procedure normally takes 60 to 120mins.
- When you wake, you will be in a recovery area where you will be monitored to ensure you recover well immediately post-operation.
- You will then return to the ward where you will be assessed by the therapy team the following day.
- Your pain relief will be reviewed and optimised following the surgery to facilitate transfers and mobility.
What will happen after hip surgery?
Following your operation, you will wake up in the post-anaesthetic care unit where the healthcare team will monitor you following your surgery. You will then be transferred back to the ward for further monitoring.
Physiotherapy
The rehabilitation routine has four components: transfer training, gait training, therapeutic exercise and practising activities of daily living.
You will work with the physiotherapists, occupational therapists, exercise practitioners and therapy assistants daily whilst in hospital. The National Institute for Health & Care Excellence (NICE) recommends that mobilisation should start as early as possible, no later than the day after hip surgery (NICE, 2012). The research evidence also shows that early mobilisation following hip fracture surgery is associated with improved patient outcomes (Agarwal et al, 2024). Therefore, if medically stable following the surgery, the therapy team aim to assess and mobilise you within 24 hours of your operation. This may be sitting on the edge of the bed or transferring into a chair using equipment.
Your weight bearing status will be decided by the consultant surgeon. You may be allowed to mobilise full weight bearing, non-weight bearing or protected weight-bearing on the affected limb. This will be explained further by the therapy team and demonstrations given.
You will likely need a transfer or walking aid initially when mobilising, but the therapy team will progress you as appropriate. The overall aim is for you to return to your pre-injury level of mobility and activities of daily living.
The therapists will look at:
- Sensation
- Blood flow to the limb
- Range of movement
- Muscle strength
- Functional movement
- Establishing a safe transfer method using appropriate mobility aids (e.g. wheeled zimmer frame, elbow crutches).
Safe technique to stand/sit
- When standing, take the majority of the weight through your ‘good’ leg and push up from the bed/chair with your arms, gain your balance and then take hold of the walking aid.
- If you are using moving and handling equipment, you can pull up on this as instructed.
- Do not pull up on walking aids, as they are unstable and can tip over.

- When sitting, wait until you can feel the chair on the back of your legs and then reach for the chair arms. As you sit down, slide your operated leg out and slowly lower yourself down.
There is a range of aids used on the wards to help facilitate patients transfer and mobilise. Some aids (e.g. hoist/sara stedy/molift) assist you in transferring and reduce the need for stepping. These might be used if you are in a lot of pain. Other mobility aids include wheeled zimmer frames, gutter frames and elbow crutches. Your therapist will assess which mobility aid will be the safest and most appropriate for you to use.
When mobilising, the following sequence should be used:
- Move the walking aid slightly ahead of you. Ensure the whole aid is on the floor.
- Step your operated leg forward and push down through the mobility aid with your arms.
- Move your good leg forward so that it is in line with your operated leg.
To aid in your rehabilitation, it is important that you continue with the exercises shown previously. Your therapy team will also advise you of further exercises to complete.
Prior to discharge, if you are going home, the therapy team will complete a step/stair assessment (where applicable) with you to ensure you are able to manage this safely prior to leaving the hospital. If you cannot manage this, don’t worry – there are other options we can discuss.
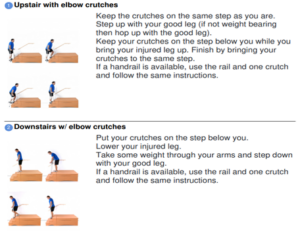
There is a simple sequence to help with the step/stairs.
Occupational therapy
Occupational therapists focus more on the functional activities of daily living (ADL) that are important to you. This includes assessing your ability to complete tasks such as bed transfers, chair and toilet transfers, personal care, dressing, meal and drink preparation.
If you are struggling with your ADL following your operation, there are techniques and various pieces of equipment that can be used to facilitate independence.
Examples of equipment occupational therapists use to facilitate independence in ADL post-operation include but not limited to the following:
- Toileting equipment (such as toilet seat frame combined, raised toilet seat and commode)
- Personal care equipment (such as perching stool/shower stool, small dressing aids like sock aids, long handle shoehorn)
- Bed transfer equipment (such as bed stick, bed lever, leg lifter) as seen in the images below.
 |
 |
 |
| Toilet seat frame combined | Perching stool | Leg lifter |
Source: TCES community
If you are unable to mobilise using walking aids, you may need to be discharged using a moving and handling tool such as a molift, sara stedy or mobile full hoist. An occupational therapist may need to complete an access visit to your property to assess your home environment with the aim of:
- determining suitability of the environment in meeting your present needs
- making necessary recommendations in collaboration with you and your family
- ensuring safety and independence as much as possible.
Recovery
Following surgery, the average length of hospital stay is approximately 5 days, however this can vary depending on your recovery.
- Day 1: mobilise with therapists using transfer or mobility aids. You will be given advice on the type of exercises to complete to improve your strength.
- Day 2 to 4: progress mobility distance aiming for independence.
- Day 5: stair assessment (if necessary), potentially get discharged from hospital.
- 2 to 6 weeks: pain continues to subside, mobility independence and distance continues to improve.
- 6 weeks: potentially return to work (if applicable) and completing activities of daily living.
- 4 to 6 months: you should have hopefully returned to your pre-injury level of mobility/function.
Everybody recovers at different speeds which is influenced by your general health and wellbeing before your injury, the nature of your surgery, and other individual factors.
Discharge from hospital
The therapy team will liaise with you and your family (where appropriate) throughout your hospital stay to discuss the options available to facilitate a safe discharge. When the doctors deem you medically fit to leave hospital, the healthcare team will make the appropriate onwards referrals depending on your individual needs.
Examples include:
- Home with equipment/support
- Rehabilitation bed (short-term rehabilitation service)
- If discharge home or to a rehabilitation bed are not suitable for your needs, the ward team will involve social services to support in making the right decision for you.
Once a decision has been made, the healthcare team will organise your discharge.
Referrals
Following your discharge from hospital, you may require ongoing therapy input. If you consent, the therapy team will make the relevant referrals to help you progress back to your baseline. Examples include:
- RAFT – rapid access, falls and trauma therapies
- Community rehabilitation physiotherapy/occupational therapy
- MSK – musculoskeletal outpatient therapy
You may also have a follow-up appointment with the consultant. This will be specified in your post-operative note and you should receive an appointment letter through the post.
Contact Numbers
Should you have any questions or would like further advice on the information contained in this leaflet, please do not hesitate to contact the trauma orthopaedic wards via telephone:
Ward 12, Hull Royal Infirmary: tel: 01482 675012
Ward 120, Hull Royal Infirmary: tel: 01482 675120
Visiting Hours: Open visiting between 11am-7pm
Useful Community Numbers
City Health Care Partnership: tel: 01482 247111 (for rehabilitation, ask for the community rehabilitation/intermediate care team)
Social Services (Hull): tel: 01482 300300
Social Services (East Riding): tel: 01482 393939
Medequip (Equipment Service): tel: 01482 249057
British Red Cross: tel: 01482 499837
Home from Hospital: tel: 01482 447673
Voluntary community and social enterprises (VCSE) – tel: 07388715255
General Advice and Consent to Treatment
Most of your questions should have been answered by this leaflet but remember that this is only a starting point for discussion with the healthcare team.
Before any member of the healthcare team examines or treats you, they must seek your consent. To make an informed decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, your information will be shared between members of the healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health or social organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns, please ask your healthcare team caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You. www.hey.nhs.uk/privacy/data-protection
If you or your carer needs information about your health, care or treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.
This leaflet was produced by the Orthopaedic Department at Hull Royal Infirmary, NHS Humber Health Partnership and will be reviewed in 3 years from publication.
Your feedback matters to us…
To ensure we deliver a safe and quality service and to help us understand the experience you have of the care you receive from our staff we would value your thoughts about the service you received.
You may be contacted as part of our quality assurance programme which is where we visit our teams and staff and talk to them about the care they provide to our patients or at any time during or after you have needed our services.
To collect this feedback, we would contact you using the registered telephone number we hold in your care record. This feedback will be strictly anonymous and whilst we will share the feedback as part of the process, we will not share any details which may identify you.
We will never ask you any personal questions about your health during these telephone calls.
If you do not wish to speak to us, please say this when we call, we do not want you to feel pressured.
References:
Agarwal, N., Feng, T., Macullich, A., Duckworth, A., & Clement, N. (2024). Early mobilisation after hip fracture surgery is associated with improved patient outcomes: A systematic review and meta-analysis. Musculoskeletal care, e1863. https://doi.org/10.1002/msc.1863
National Institute for Health and Care Excellence (2012): Hip Fracture in Adults. Available at: Quality statement 6: Rehabilitation after surgery | Hip fracture in adults | Quality standards | NICE [Accessed 30th May 2025]
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

