- Reference Number: HEY231/2025
- Departments: Emergency Department, Physiotherapy
- Last Updated: 30 June 2025
Introduction
This leaflet has been produced to give you general information about your injury. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
What is a Calf Strain?
There are two muscles in the back of the lower leg that combine to form the calf. These are called the gastrocnemius, which is the big muscle at the back of the lower leg and the soleus muscle, which is a smaller muscle lower down in the leg. A calf strain occurs when small portion of either of these two muscles is torn. It is a common injury and is often caused by overstretching or by putting excess force through the calf muscle.
What are the symptoms?
Your symptoms may vary depending on the severity of your calf strain. Symptoms commonly include:
- Sudden, sharp pain in the back of the leg
- Pain, swelling or bruising in the calf muscle
- Difficulty or pain when standing on your toes
What if I need pain relief?
To manage your pain, over the counter pain relief can be taken such as paracetamol or ibuprofen gel.
However, if you have allergies or conditions which prevent the use of pain relieving or anti-inflammatory medication or are taking medication(s) for other conditions. Please seek advice from your doctor or a pharmacist before taking any pain relief.
What should I do in the first 72 hours after the injury?
Initial treatment aims to control the pain and swelling in the calf by following the PRICE principle.
P Protection – The use of supportive shoes/trainers will help to protect and support the calf. Trainers or sensible shoes with a slight heel raise will help prevent overstretching the calf in the first few days.
R Rest –
Rest from activity for the first 72 hours is recommended. However, complete rest is not advised. You may be provided with crutches to take weight off the injured calf or a small heel wedge which will prevent overstretching of the calf and help healing.
Gentle movements should be practiced, however they should be pain free. Initially, you may find that the ankle does not move far but this will improve as you practice the exercises. You should practice these exercises 10 times, 3 to 4 times per day.
| 1.In sitting, pull your toes and ankle up towards you.
To assist this movement, place a scarf or towel around your foot and gently pull your foot up, by pulling the scarf with your hands. Hold this position for five seconds. |
 |
| Now point your toes away from you and hold for five seconds. |  |
| 2.While lying or sitting put a scarf around your foot and gently bend and straighten your knee. |  |
I Ice –
Ice will help reduce the pain in your calf and so should be applied for 15 – 20 minutes before performing the exercises above. This will help to reduce the swelling.
There are many different ways in which ice can be applied however it believed crushed ice, in the form of frozen peas for example, is the most effective. Whichever method you choose it is important that you wrap the ice in a damp towel, in order to prevent it from ‘burning’ the skin.
Please Note:
- Only use an ice pack on areas that have normal skin sensation i.e. where you can feel hot and cold
- Do not apply ice to an open wound
- Do not apply an ice pack to an area that has poor circulation
- When you apply ice to your skin, check the skin every five minutes and stop using it if:
- the area becomes white, blue or blotchy
- the area becomes excessively painful, numb or tingles
C Compression –
Compression is used to control the swelling and support the calf. You may have been given a tubigrip bandage to help control the swelling.
The tubigrip should be removed if you develop any signs of poor circulation such as tingling, numbness, blueness of the foot and increasing pain. It should also be removed whilst you are asleep as you cannot monitor for these symptoms.
E Elevation –
The leg should be elevated above the heart for as much as possible and you should avoid long periods where the leg is not elevated. This will help to reduce and prevent the swelling of the calf.
What not to do
Consuming alcohol, massaging the injured area and applying heat can all be detrimental in the early stages of healing and therefore should be avoided in the first 72 hours. It is important to note that smoking may also delay the healing process
For further advice on stopping smoking, please see the ‘Quit smoking’ information page on the NHS website or use the QR code below.
Rehabilitation and recovery
After 2 weeks, most sprains will be feeling better. However, you should avoid strenuous exercise for up to 8 weeks to reduce the risk of further injury. Everyone recovers from injuries at different rates, and your recovery is dependent on the severity of the injury and the presence of any other medical problems.
The following exercises which will help you to regain full function, flexibility and strength. Begin these exercises once your pain has settled and you no longer require crutches, if you were provided them. When doing these exercises you should stop when you are at the point when it becomes painful. We do not recommend you push into the pain as the injured tissue is still healing and over stretching can delay the healing.
Exercises
|
|
 |
Keep this leg straight with your toes pointing forward and the heel on the floor.
Now bend your other knee until you feel a stretch in the calf of your injured leg. Hold this for 30 seconds and repeat three times per day. |
|
|
 |
Ensure that your toes point forward and bend both knees, keeping the heel of your injured leg on the floor.
You should feel a stretch in the calf of your injured leg. Hold for 30 seconds and repeat three times per day. |
Stand holding on to a chair, spread your weight equally over both feet and push up onto your toes as high as possible. |
|
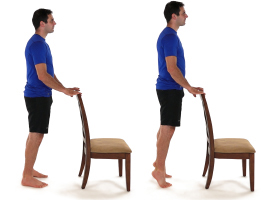 |
Hold for five seconds and slowly lower. Repeat 10 times, twice per day.
Once this becomes easier you can increase the number of repetitions or progress to repeating this stood on the injured leg on its own. |
All photos with kind permission of ©Physiotec™
When can I return to normal activities?
If you participate in an active hobby then it is advisable that you do not return to this until you have full strength, full range of movement and you can walk briskly without experiencing pain and swelling.
If you play a sport, you can practice sports specific activities; like dribbling or jumping. Build up these exercises gradually, in order to help regain strength and flexibility, before returning to full training sessions and competition.
Do I require further treatment?
You may be advised that you require physiotherapy following this type of injury, unless your symptoms are minimal on your initial appointment. Your physiotherapy could be at a variety of locations in the Hull and East Riding area.
You can self-refer to physiotherapy by contacting the following number depending on the location of your doctor:
- Hull GP patients self-refer to Healthshare: tel: 01482 300003
- East Riding GP patients self-refer to East Riding Physiodirect: tel: 01377 208300 or self-refer online at chcpmsk.org.uk
On occasions the clinician may wish to refer you to the physiotherapy team within the hospital trust. If this is the case they will advise you of this and you should receive an appointment at Hull Royal or Castle Hill Hospitals within 5 to 7 days of your attendance at the Emergency Department. If you have received no contact within this time please call the physiotherapy admin team on tel: 01482 674880.
When to seek further help
If 10 days following your injury you are unable to weight bear and the calf remains painful and swollen, despite following the advice in this leaflet, please contact the physiotherapy team that you were advised to contact in the section above.
Please be aware it is very important that you see your doctor immediately if, after following advice in this leaflet, your symptoms do not improve and you notice that the calf becomes increasingly tender, red and that it is tender and hot to touch.

