- Reference Number: HEY997/2025
- Departments: Haematology, Oncology (Cancer Services)
- Last Updated: 30 November 2025
Introduction
This leaflet has been produced to give you general information about your condition and its treatment. Many of your questions should be answered by this leaflet. If, after reading it, you have any concerns or require further explanation, you will have the opportunity to discuss this with the health professional involved in your care.
What is an Unsuspected Pulmonary Embolism?
An unsuspected or incidental pulmonary embolism is a small blood clot in the lungs, diagnosed following a computed tomography (CT) scan that was done for other reasons. Most patients who have them do not know they have one because these blood clots are usually too small to cause any symptoms.
If these blood clots are left untreated, they can grow and start causing symptoms that, in some cases, can be troublesome, such as shortness of breath and fatigue. There is also a risk of embolic events if part of the clot breaks off.
Following a diagnosis of an incidental pulmonary embolism, you will be referred for assessment by a healthcare professional in the Cancer Acute Assessment Unit (CAAU) who has specific experience in managing unsuspected pulmonary embolisms.
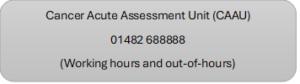
The assessment may take place on the same day as your scan, or it might be done the next working day. However, if you feel unusually breathless or unwell after your scan, please contact the CAAU triage number. You will be advised on what to do next.
What will happen during the assessment?
An anticoagulant, a medicine that thins the blood, is used to treat an unsuspected or incidental pulmonary embolism.
Anticoagulants can be given in several different ways:
- A heparin-based blood thinner that is injected under the skin may be prescribed, and you may leave the hospital with a supply of pre-filled syringes for you to inject yourself daily at home. The nurse undertaking your assessment will show you how to do this yourself.
- Rivaroxaban is a tablet that you will initially need to take twice a day for three weeks and then just once a day for the duration of the treatment. Another blood thinner in the same category is Apixaban, taken twice daily. These tablets do not need regular blood tests for monitoring.
- Warfarin is a blood-thinning tablet that takes several days to become effective, and regular blood tests are required to ensure the correct dose is given. Routine blood tests may be needed to monitor and stabilise your warfarin levels. You may have a combination of both warfarin and LMWH.
The healthcare professional involved in your care will inform you of the treatment you will be receiving.
In the rare case that you are already on an anticoagulant, the team will decide whether to adjust your dose or switch anticoagulants, depending on your specific circumstances.
Can there be any complications or risks?
As you receive a medicine to make your blood thinner, you may notice that you bruise more easily. Any bleeding, for example, if you accidentally cut yourself or have a nosebleed, will be heavier than normal.
If you are injecting a heparin-based blood thinner, you may notice bruising around the injection site. This is normal and usually not something to be concerned about. You can help prevent this by touching the injection site as little as possible during and after the injection is given.
Serious bleeding is uncommon (less than 5%). If you experience any bleeding that you cannot control or explain, or notice soft, black, tarry stools, you should report to the Emergency Department of your nearest hospital.
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so they can offer support. There may be information they need to know, especially if they are taking care of you following the assessment.
What happens afterwards?
Following your assessment, if you are treated as an outpatient, you will receive a month’s supply of your medication and an information pack.
You will need a repeat blood test 7 days after starting LMWH and will be given a follow-up appointment to see your consultant.
If you are admitted, treatment will be initiated on the ward. The expected length of stay will depend on your condition. On discharge, you will be given a small supply of medication and a follow-up appointment to see your consultant.
Your consultant will advise you on how long you need to take your medication; however, the length of treatment is usually 6 months, but can vary according to your circumstances.
Future prescriptions for your medication should be obtained from your GP.
Please do not hesitate to contact us if you require further advice about the issues in this leaflet.
24-hour hotline: