- Reference Number: HEY1596/2025
- Departments: Physiotherapy, Therapies
- Last Updated: 30 September 2025
MSK Outpatient Services Hull Royal Infirmary
Introduction
This leaflet has been produced to give you general information following your recent guided hip injection. It is intended to support your recovery and explain the next steps in your rehabilitation. Most of your questions should be answered in this leaflet, but if you have any further concerns, please contact your GP or the physiotherapy team.
What is a Guided Hip Injection?
A guided hip injection is a procedure where medication is delivered directly into the hip area using imaging (such as ultrasound) to guide accurate placement. It is used to help reduce inflammation and relieve pain.
Why do I need Physiotherapy?
Following your injection, physiotherapy can help restore your movement, strength and function. It supports your recovery by guiding you through a personalised exercise plan and helping prevent further stiffness or loss of mobility.
How do I refer to physiotherapy?
You are encouraged to self-refer to physiotherapy for continued care. Please refer based on your GP’s location:
If you have an East Riding GP:
Contact the City Health Care Partnership (CHCP) MSK physiotherapy Team:
- Phone: Tel: 01377 208300
- Online: www.chcpmsk.org.uk/self-referral-form-introduction
If you have a Hull GP:
Contact the Physiotherapy Department at Hull Royal Infirmary:
- Phone: Tel: 01482 674880
Please state the reason for your referral when contacting the team. You will be added to the appropriate waiting list and contacted to arrange an appointment.
What happen afterwards?
You may begin gentle exercises 2 to 3 days after your injection to help settle any initial discomfort or flare up. These exercises are important for maintaining joint mobility and preventing stiffness.
Exercise Guide
Please start gradually and only complete exercises that feel comfortable. Stop if you experience pain.
Hip Abduction side lying

Lie on your side with your head supported. Bend lower leg. Lift the top leg up a small amount (about a third of the way up), keeping your leg in line with your body. Do not move the leg forwards. Do the exercises 5 to 10 times, repeat 1 to 2 times, do once or twice a day, hold each movement for 5 seconds.
Alternatively, you can do this exercise in standing (see next)
Standing hip Abduction

Stand upright and hold onto a chair. Move your leg out to the side without lifting your pelvis. Slowly return to the starting position. Do this exercise 5 to 10 times, repeat 1 to 2 times, do once or twice a day, hold each movement for 5 seconds.
Glute Bridge

Lie on your back with your knees bent. Tighten your buttocks and lip your hips until your body is in a straight line. Slowly lower back down. Do this exercise 5 to 10 times, repeat 1 to 2 times, do once or twice a day, hold each movement for 5 seconds
Partial Squat
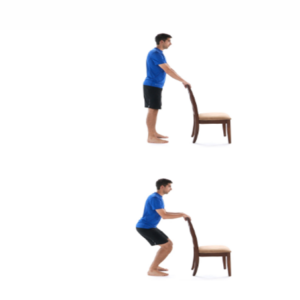
Stand holding a worktop or counter. Keep your back straight and your heels on the floor. Bend your knees slightly into a small squat, keeping your hips above knee level. Do this exercise 5 to 10 times, repeat 1 to 2 times, do once or twice a day, hold each movement for 5 seconds.
Active hip flexion and extension

Stand on one leg and hold onto a stable surface. Swing the other leg forwards and backwards, keeping the knee straight and your body steady. Do this exercise 5 to 10 times, repeat 1 to 2 times, do once or twice a day, hold each movement for 5 seconds.
All photos of exercises and instructions with kind permission of Physiotec/Wibbi
Can there be complications or risks?
Possible side effects or complications
It is common to experience a temporary flare -up of symptoms after the injection. This may include:
- Increase joint discomfort
- Swelling
- Redness
If this happens:
- Rest the joint
- Apply ice for 10 to 15 minutes (wrap ice in a towel; do not place directly on skin)
- Avoid strenuous activity
These symptoms usually settle within a few days
Contact your GP promptly if you experience:
- Persistent or worsening pain
- Redness, swelling, or warmth
- Fever
Need further advice?
If you have any questions or concerns, please contact your GP or the appropriate physiotherapy team using the contact details above.
Glossary (helpful words)
- Guided injection – An injection placed using imaging to improve accuracy.
- Inflammation – Swelling and irritation in the body that can cause pain.
- Abduction – Moving your leg away from the body.
- Physiotherapy – Treatment to help improve movement, strength, and function
- Ultrasound – A scan that uses sound waves to create images inside the body and help guide injection accurately.
- Self-referral – Contacting a healthcare service yourself without seeing your GP first.
- Flare-up – A short-term increase in pain or symptoms.
This leaflet was produced by the MSK Physiotherapy Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in September 2028.
| General Advice and Consent
Most of your questions should have been answered by this leaflet but remember that this is only a starting point for discussion with the healthcare team. Consent to treatment Before any doctor, nurse or therapist examines or treats you, they must you’re your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information. The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means: • you must be able to give your consent • you must be given enough information to enable you to make a decision • you must be acting under your own free will and not under the strong influence of another person Information about you We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data. We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you. Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You. If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged. |
Your feedback matters to us…
To ensure we deliver a safe and quality service and to help us understand the experience you have of the care you receive from our staff we would value your thoughts about the service you received.
You may be contacted as part of our quality assurance programme which is where we visit our teams and staff and talk to them about the care they provide to our patients or at any time during or after you have needed our services.
To collect this feedback, we would contact you using the registered telephone number we hold in your care record. This feedback will be strictly anonymous and whilst we will share the feedback as part of the process, we will not share any details which may identify you.
We will never ask you any personal questions about your health during these telephone calls.
If you do not wish to speak to us, please say this when we call, we do not want you to feel pressured.

