- Reference Number: HEY1086/2024
- Departments: Neurology and Neurosurgery, Physiotherapy
- Last Updated: 1 January 2024
You can translate this page by using the headphones button (bottom left) and then select the globe to change the language of the page. Need some help choosing a language? Please refer to Browsealoud Supported Voices and Languages.
Introduction
This leaflet has been produced to give you information about how to care for your back following surgery. Most of your questions should be answered by this leaflet. It is not meant to replace discussion between you and your physiotherapist or spinal surgeon, but may act as a starting point for discussion.
Your consultant spinal surgeon should have explained the operation procedure and the risks and benefits. This leaflet will concentrate on providing you with information on the physiotherapy input you can expect after surgery.
If after reading this leaflet, you require further explanation please discuss this with a member of the physiotherapy team who has been treating you.
Preparing for your operation
Before your operation it is important to prepare yourself and your home to ensure you get the best outcomes. Arrange for friends or family to help support you with things like shopping and transportation. Set up your home to make commonly used items easier to reach and use. Keep yourself as active as you are able within the limitations of your symptoms.
If you are having your operation in the Day Surgery Centre you will be invited to a telephone call with one of the physiotherapy team who will be able to give you more advice.
Physiotherapy after surgery
You will be reviewed by the physiotherapist either on the day of your surgery or the first day after your surgery.
The physiotherapist will assess your limb movement and sensation and will teach you exercises (which are described later in this leaflet) to help you to get your back moving.
The physiotherapist will also teach you how to get out of bed and encourage you to begin walking. You may have some attachments such as drips, catheter and drains. These do not stop you from walking, although you may need some help at first.
You will also be expected to sit out into a chair for short periods from the day of surgery.
In some cases you may be assessed shortly after surgery to help you to prepare for discharge home on the same day. Your consultant will have discussed with you before your surgery if you are likely to be a day case patient. If you are going home on the same day of your surgery you will need to have someone at home with you overnight.
General advice
The best thing you can do for your back is to try to relax it and move it as freely and normally as possible. However, for the first few days or weeks, after your operation it is normal for your back to initially be stiff and sore. During this time you may find yourself bracing and protecting/guarding your spine as you move about. It is a common belief that bracing and tensing your spine will protect it but in fact this often does the opposite and creates more pressure and can lead to ongoing discomfort.
It is important to remember that as things begin to heal and the pain settles down you should try to move freely and confidently again. Following your operation you should aim to get back to normal levels of activity in a graded manner. This can start straight away by sitting up in bed, sitting out in the chair and taking short walks. You should try to avoid long periods where your back is inactive.
It is important to strike a balance between periods of activity and rest. Inactivity can be just as harmful to your back as over activity.
Lying
The most important thing when you are lying down is that you are comfortable. Some people prefer harder mattresses and others softer mattresses; you should be guided by comfort and pick what suits you.
You are free to move around in bed and practising rolling from side to side will make getting in and out of bed much easier.
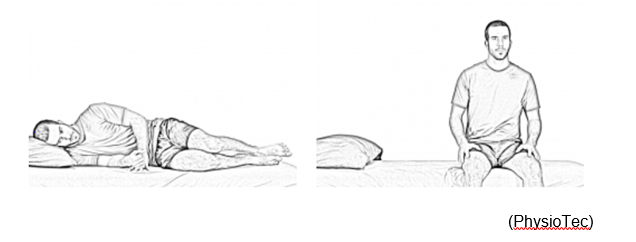
It is important to minimise the strain on your back when getting in and out of bed. To get out of bed, roll onto your side and swing your legs over the edge of the bed whilst pushing up with your arms. Sit on the edge of the bed for a moment before standing up.
Sleeping
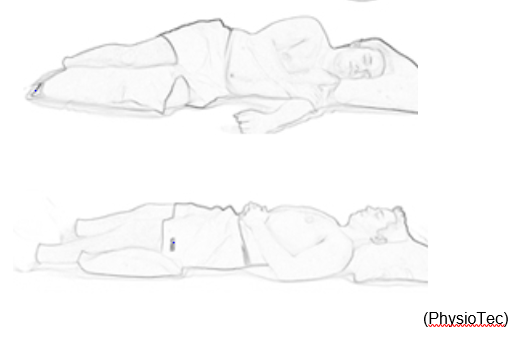
You can sleep in any position you find comfortable. Below are a couple of positions you may find comfortable.
Sitting
There is no such thing as the perfect sitting posture; this varies depending on the individual. Some people prefer to sit up straighter while others prefer sitting more slouched. You should sit in the posture that feels most comfortable. Although we have traditionally sat up straight there is no scientific evidence to support this, sitting with a more relaxed lower back is not in any way harmful.
Walking
When you first start walking your lower back may be sore, this will improve over the first few days and weeks and is to be expected. It is important to try to walk little and often and gradually build things back up to normal. Do not worry too much about holding an upright posture; you are best to try to walk as normally as possible.
Personal hygiene
To begin with you should try to keep your wound dry, this is made easier by showering rather than having a bath. If you have any concerns about washing then please discuss this with the ward occupational therapist before you are discharged home.
You should keep the wound dry until your clips/stitches are removed. The nursing staff will update your discharge letter with the date your clips/stitches are due out and this will be sent to your doctor. Call your doctor to arrange an appointment for these to be removed on the date given on the discharge letter. These are usually removed by your doctor’s practice nurse.
Discharge home
Prior to being discharged from hospital you will need to be able to complete your exercises, walk short distances comfortably and be able to walk up and down a flight of stairs (if you have them at home).
It is your responsibility to continue with your exercises and back care independently and liaise with your doctor if necessary.
If you continue to have any pain, stiffness or weakness you may be referred for ongoing physiotherapy at your local physiotherapy unit.
Please monitor your wound for any signs of infection. These include leaking, redness and swelling. If you develop any of these symptoms you should call the ward or your local doctor for advice.
You must wear your Thrombo-Embolic Deterrent (TED) stockings for 2 weeks from your discharge from hospital. These will reduce your risk of developing blood clots after your operation; they should be removed for bathing/showering then put back on once your legs are dry. After this time you can remove your TEDs. The nursing staff will provide you with more information regarding TED stockings on your discharge from hospital.
Pain Management
Following your surgery it is normal for you to experience some pain and discomfort as you recover. Try not to panic about this as it is to be expected. If you are struggling with this you may need to consult with your doctor for advice. It would be better for you to take medication that allows you to gradually get back to your daily routine than to struggle and become more inactive.
Driving
Your driving/sitting posture should be based on comfort (please see the previous guidance on sitting). You should gradually build your sitting tolerance back up over time and take regular breaks when driving long distances where you get up and move about.
It is your responsibility to ensure your vehicle insurance covers you to drive prior to commencing driving after your surgery.
Lifting
Avoid lifting heavy objects and also holding items at arms length away from your body. Always use a correct lifting technique, bending at the knees and not at your back (see following diagram). Avoid bending, twisting or leaning movements.

Work
Return to work will depend very much upon your recovery and the type of work you do. It is important that you discuss with your doctor when it is safe to return to work.
Exercise
Exercising your back can help provide pain relief and assist the healing process. It is best to keep moving little and often and start by moving gently to begin with. Try to relax when moving rather than tensing up, as this often makes things stiffer. It may be painful to begin with but this is to be expected after an operation. If this is the case you should keep moving but focus on smaller movements and make sure you keep movements relaxed.
- Relaxation breathing (abdominal breathing). Laying down, put one hand on your upper chest and one hand on your tummy just below your rib cage. Relax the shoulders and hands. As you breathe in, allow the abdomen to rise and as you breathe out, allow the abdomen to flatten. There should be little or no movement in the chest. Try to slow your breathing down. Using this exercise often helps decrease muscle tension and relieves pain.
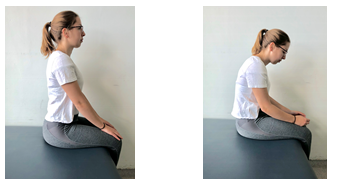
- Sat over the edge of the bed or in a chair gently practice moving from sitting up straight down into slouching. Repeat this process smoothly little and often. This creates some gentle straightening and bending in your lower back and will help get you moving more freely again.
- Lie on your back with your knees bent. Activate your lower abdominals (tummy muscles) by bringing your belly button inward and by squeezing your pelvic floor muscles. Maintain steady abdominal breathing while tilting your pelvis and flattening your back to the ground. Return slowly to the starting position and then arch your back, tilting your pelvis in the opposite direction. Return to neutral and repeat, aiming for 3 sets of 10.
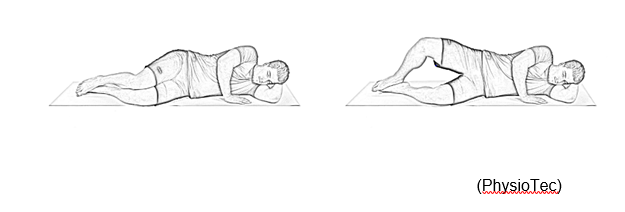
 Lie on your side with both legs slightly bent. Lift your top leg, keeping your hips stable, your leg slightly bent and your heels together. Rotate your hip so that your foot and your knee cap are pointing upward during the movement, be careful not to start falling backwards. Return to the starting position and repeat. Try to do 5 sets, then 10 sets, trying to hold for 5 seconds on the left side then 5 seconds on the right side.
Lie on your side with both legs slightly bent. Lift your top leg, keeping your hips stable, your leg slightly bent and your heels together. Rotate your hip so that your foot and your knee cap are pointing upward during the movement, be careful not to start falling backwards. Return to the starting position and repeat. Try to do 5 sets, then 10 sets, trying to hold for 5 seconds on the left side then 5 seconds on the right side.
- Walking little and often after your operation will be very useful. Build your walking up slowly depending on how you are feeling. There is no set distance or time you should be walking but try to build this gradually in the weeks following your operation.
Day surgery patients Castle Hill Hospital
Please urgently contact the appropriate number below if you have any of these problems when you go home.
- New post-operative numbness or a loss of sensation in the arms or legs.
- New post-operative weakness in the arms or legs.
- New bladder or bowel dysfunction (changes in the way your bladder and/or bowel are working).
- Fluid discharge/bleeding that is leaking outside of your surgical dressing.
Monday-Friday 08:00 to 18:00 hrs – Contact physiotherapists on ward 9 at Castle Hill Hospital on Tel. 01482623009. Please ensure you ask to speak to the Physiotherapy team directly.
Monday-Friday 18:00 until 08:00 hrs or Saturday and Sunday – Contact Ward 4 at Hull Royal Infirmary on Tel. 01482675004.
Telephone follow-up service
Your consultant may place you onto the telephone follow-up service. This is when you are expected to recover well with time and you do not routinely need to see the consultant for follow-up review.
If you are in the telephone follow up service you will receive an appointment through the post for someone to call you between 6 to 8 weeks after your operation. Please contact the ward you were discharged from to discuss your follow up if you have not received an appointment by 6 weeks after your surgery.
PLEASE REMEMBER THAT YOU DO NOT HAVE TO ATTEND THE HOSPITAL FOR THIS APPOINTMENT, THIS IS A TELEPHONE CALL ONLY.
Should you require further advice on the issues contained in this leaflet, or you need to contact us, please telephone the hospital where your surgery took place.
- Castle Hill Hospital – Ward 9 – Tel: 01482623009
- Hull Royal Infirmary, Physiotherapy Department (ask for Neurosurgical Physiotherapists) – Tel: 01482674539
- Hull Royal Infirmary, Ward 4 – Tel: 01482675004

