When you don an NHS Security uniform you never know what you’re going to be dealing with next.
One minute you could be answering a parking permit query and the next you’re saving someone who is attempting to take their own life.
You’re no sooner back at the office when you get a call to say there’s an issue with anti-social behaviour and then you’re rushing to the aid of frightened staff on a ward, where a patient has become violent, and they need your assistance in keeping everyone safe.
And that’s all in the space of one shift, with little time to pause or reflect on what you have just dealt with before the next call comes in.
Even if you do get some time in the control room, you’ll likely be dealing with queries from the public, monitoring CCTV or pulling CCTV footage to hand to the police as evidence.
In fact, the only thing you can be sure of is that you will be busy from the moment you walk through the door.
We recently caught up with some of our Security Officers across NHS Humber Health Partnership to find out more about life on the front line of protecting patients, staff and visitors across our hospitals.
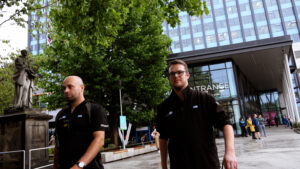
- Security Team Leader Robert Marvell
- Security Supervisor Tristan Kenny
A ‘typical’ day
You don’t need to spend long talking to our Security teams before you know that there’s not really such a thing as a typical day.
Yes, they have day-to-day tasks, such as monitoring CCTV, patrolling our sites, providing a reassuring presence, and calling into our wards and departments to check everything’s okay.
But when issues arise, they’re the first port of call – particularly if someone has become violent and, sadly, if weapons are involved.
Our teams in both Northern Lincolnshire and Goole NHS Foundation Trust and Hull University Teaching Hospitals NHS Trust said they’d had to deal with people with knives, needles and even what staff had feared was a gun but turned out to be a high-powered and very realistic looking air gun.
Rob said: “Three or four months ago, during a night shift, we got called up to a ward and told a patient was hidden behind a door with a weapon.
“We’ve gone up with our body cameras active and opened the door to be confronted by a patient who has ripped off the big blue bar from the wall of the disabled toilet.
“As we took control of the patient, they swung and me and hit me twice. The first time, luckily, hit my stab jacket but the second one hit me in the arm. I have a scar.
“It’s not what I want to do but I’d rather it be me than a doctor or a nurse, because I am here to keep them safe.”
Mental strain
Increasingly, the incidents the teams deal with are linked to drugs, alcohol, or mental health issues but, whatever the cause, the team are quickly on hand.
Only recently in Hull, the team found a patient in the toilet with a ligature around their neck. The Security officer managed to get their hand down to pull the ligature off their neck, saving their life.
Unfortunately, this is far from an isolated incident. Both teams talked about numerous occasions when they have been called to deal with people threatening to take their own lives – including many where they have had to physically intervene.
Rob said: “We are trained to deal with the matter at hand and whatever comes after it, but some people think that because I turn up and I have a radio and a stab jacket on, and we’re used to dealing with people who are extremely aggressive, that we’re robots. But I am not a robot. I have a family at home, I bleed and hurt like everybody else.
“When you’re at work you get in the mindset of ‘it’s work’ and you do it but when you get home, sometimes you sit back and like *whistles* “Have I really dealt with that?”
“You also have to have pretty thick skin. You get people making threats to your family, you, your job – but we try not to take it personally. They don’t have an issue with me. They don’t know me. It’s directed at the uniform.”
Tristan said his former career in the Army and debriefing incidents with colleagues had helped him to cope with the demands of the role, adding: “We’re here to provide safety and reassurance for everyone on the site – whether it be a patient, a visitor, a member of staff – anybody really.
“I like to break things down. I divide my day into meal times – whatever happens after breakfast is going to happen but it’s not going to last until lunch – and then I am going to have my lunch and the next thing isn’t going to happen until after that.
“All of a sudden I’m in bed and I’ve not got a whole day’s worth of stuff – I’ve just got that bit between breakfast and lunch.
Powerful language
Talking isn’t just a coping mechanism for the teams, it’s a valuable tool in managing incidents.
Tristan said: “Sometimes you find yourself just listening and a lot of the time that makes people feel heard. Then they feel that they’ve been taken seriously and, all of a sudden, they calm down without even realising it.
“One incident that comes to mind was an elderly patient who came into A&E and, unfortunately for everyone involved, was wielding some kitchen knives at the reception staff.
“I was the first one to arrive on scene and there was an elderly patient holding three knives in one hand. One of them was a bread knife.
“They’d come in seeking help. I don’t know what other avenues they’d explored prior to that but they seemed absolutely desperate to get help and seemed to think that this was their last resort.
“After speaking to them for a little while they calmed down and I deescalated the situation. They put down the knives and we were able to pass them through the security screen and remove them from the situation.
“We actually managed to get them booked in after that. I think everyone present could see it was just a confused elderly person – a sort of cry for help – and, in the end it was a really positive outcome and they got the help they needed.”
Juggling priorities

Good communication is also a key factor in helping the teams to prioritise when there are multiple incidents happening at the same time.
When this is the case, the teams need as much information as possible to assess where it’s most important for them to attend, based on the level of potential risk to everyone involved.
It’s a really comprehensive assessment, ensuring that the teams are deployed where they are needed most, that there are enough of them to deal with the situation, they have the right equipment and – if needed, that emergency services are also alerted.
So, while it can be frustrating if you need your permit query answering or you’re locked out of a room and the team are tied up, you can rest assured it’s for good reason.
Rewarding work
While NHS Security is a challenging role, it’s also one that the teams find extremely rewarding whether it’s the joy making people laugh and feel a little better while they’re helping to deal with their query or the satisfaction of a job well done.
Tristan said: “It is rewarding to see the other side of people who have been lashing out when they come out.
“They’ve had something wrong with them that’s caused that behaviour and then, they’ve got themselves settled and they’re better. All of a sudden you have got a random patient you have been dealing with for days and they’re apologising to you.”
Rob added: “Working for the NHS is probably my proudest achievement. I am proud to come to work, put on my uniform and go home at the end of my shift knowing that everything has been dealt with safely – that everyone’s happy and that they have gone home safe.
“That’s all I can ask for and I am proud to be a part of the NHS”.